A recent study has determined the use of 3D printing and imaging reduces complications in robotic surgeries for the treatment of prostate cancer.
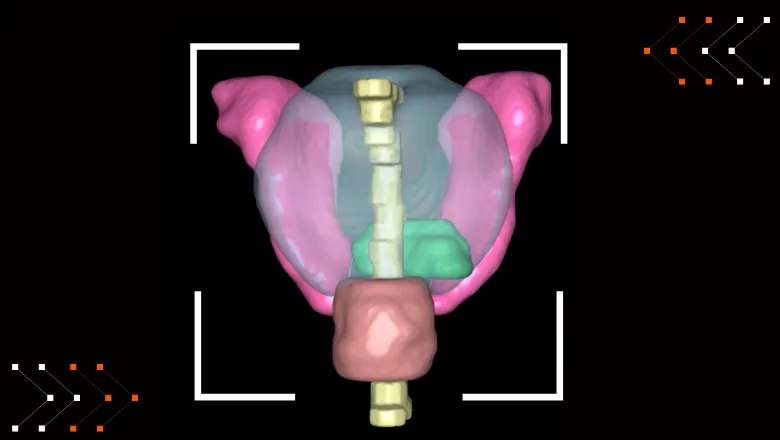
Prostate Cancer is often treated by a robotic keyhole surgery called a robotic-assisted radical prostatectomy. Accompanying this surgery is an MRI scan which tells the surgeon where the cancer is within the prostate.
Currently, surgeons are expected to mentally reconstruct a patient's 3D anatomy from the 2D imaging presented to them. This reconstruction becomes less challenging with experience, although it remains an issue for junior surgeons and in difficult cases.
Researchers from King's College London, Guy's and St Thomas' NHS Foundation Trust, Innersight Labs, Nvidia, and San Raffaele Hospital, have investigated current evidence and trends on the effects 3D models have in the reduction of complications resulting from surgery. The results suggest that cancer lesion outcomes improve, while there is not enough evidence to conclude an improvement on functional outcomes such as urinary incontinence and erectile disfunction.
Our research has identified that the use of 3D-printed technology is most effective during a robotic radical prostatectomy. It allows surgeons to operate more precisely, and successfully remove the prostate cancer while reducing damage to the sphincter muscle and nerve bundles. The operation is thus personalised to the individual patient while reducing the complications of surgery.
Prof Prokar Dasguptar OBE, King's Health Partners Professor of Surgery
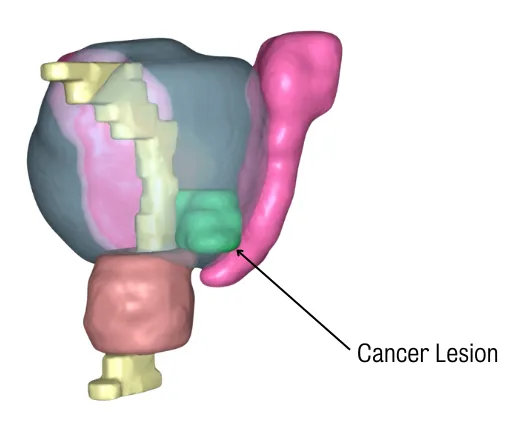
Alongside these findings, researchers are using Artificial Intelligence to map the prostate with the cancer on MRI scans, speeding up the creation of 3D models in future studies. The results are used to 3D print the prostate and create a 3D image on a computer screen for surgeons to refer to during the robotic procedure.
We are currently running a feasibility study at Guy's Hospital that is allowing us to introduce state-of-the-art technology for the automated segmentation of prostate anatomy using Artificial Intelligence and the automated generation of 3D printed/virtual patient-specific models, while designing more sophisticated algorithms that could further reduce surgical complications.
Dr Alejandro Granados, Principal Investigator and Lecturer in Surgical Data Science, School of Biomedical Engineering
Future studies are expected to investigate the effects of 3D models on surgical outcomes across different levels of surgeons' experience.
This work was supported by The Urology Foundation, The John Black Charitable Foundation, core funding from the Wellcome/EPSRC Centre for Medical Engineering and The Dr Recordati Surgical Data Science Programme.








