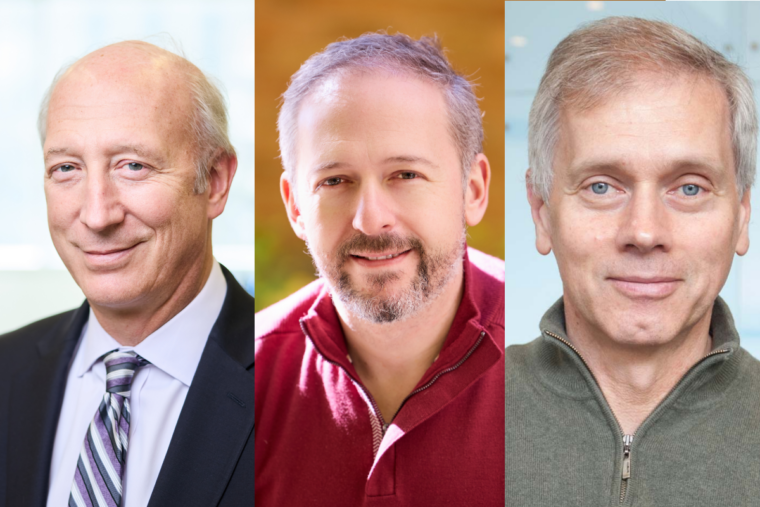
Washington University School of Medicine in St. Louis has received a three-year $4.5 million grant from the Carol and Gene Ludwig Family Foundation, aimed at advancing research on neuroimmunology and neurodegeneration with the ultimate goal of developing new treatments for Alzheimer's disease. Administered by WashU Medicine's Brain Immunology & Glia (BIG) Center, the Carol and Gene Ludwig Initiative in Neuroimmunology Research will support innovative projects led by David M. Holtzman, MD; Jonathan Kipnis, PhD; and Marco Colonna, MD, in addition to other faculty members through a seed grant program.
"This award recognizes exceptionally exciting and innovative work in the area of neuroimmunology at WashU Medicine," said David H. Perlmutter, MD, the George and Carol Bauer Dean of WashU Medicine, executive vice chancellor for medical affairs and the Spencer T. and Ann W. Olin Distinguished Professor. "This support from the Ludwig Foundation will help to accelerate advances in understanding the interplay between the brain and the immune system and harness that knowledge to identify novel targets for treatment of Alzheimer's disease and possibly even prevention of dementia. This work is among the finest examples of the secret sauce of collaboration at WashU that brings together physicians and scientists from different disciplines to achieve more than they could individually."
Holtzman, the Barbara Burton and Reuben M. Morriss III Distinguished Professor of Neurology, contributed to understanding the role for the immune system in Alzheimer's disease, in work published in Nature in 2023. The brain's resident immune cells - microglia - had been previously implicated in causing injury to brain tissue. The Holtzman laboratory found that microglia interact with another immune cell type - T cells - enabling them to both enter the brain and contribute to neurodegeneration in a mouse model. Their work demonstrated that removing T cells from the brain prevents brain damage and cognitive impairment.
The Carol and Gene Ludwig Initiative in Neuroimmunology Research will support an in-depth study of the processes responsible for activating and recruiting a subset of harmful T cells to the brain to cause disease.
"We know the imbalanced immune response could be involved in causing neurodegenerative disease," Holtzman said. "A complete picture of the immune players and their interactions will help us identify and test therapeutic targets to interfere with the progression of neurodegeneration."
Colonna, the Robert Rock Belliveau, MD, Professor of Pathology, in collaboration with the Holtzman lab, will explore innovative therapies that enhance microglia's ability to engulf amyloid protein plaques that accumulate in the brains of Alzheimer's patients. In research published in Science Translational Medicine, Colonna and Holtzman previously found that mobilizing microglia by lifting their natural brakes is a promising strategy for removing the noxious plaques that build up and cause cognitive decline in Alzheimer's. With the funding, they can advance this approach toward therapeutic testing.
Kipnis, the Alan A. and Edith L. Wolff Distinguished Professor of Pathology & Immunology and a BJC Investigator, studies the interactions between the immune system and the central nervous system. Studies in his lab published in Nature have shown that the drainage system in the brain physically connects the immune system with the central nervous system, opening opportunities to study the neuroimmune interactions during the course of disease and in good health. The new award will support Kipnis' endeavors to engineer immune cells to prevent or halt neurodegeneration in mouse models of Alzheimer's.
"These studies have the potential to transform the treatment of Alzheimer's," said Kipnis, the inaugural director of the BIG Center. "We aim to develop Alzheimer's immunotherapies that can be tailored to individual patients, while also expanding this work into other age-associated central nervous system disorders."
The initiative also will fund seed grants - the Carol and Gene Ludwig Awards for Neuroimmunology Research - that will be administered by the BIG Center's leadership team. Two applicants will be selected each year for three years, with $200,000 distributed each year.
The Carol and Gene Ludwig Family Foundation previously provided grant funding to WashU Medicine, including support for Holtzman and Kipnis. The charitable private foundation, established in 2002, invests in organizations that accelerate medical and scientific discovery, enable access to educational and economic opportunities for young people, and enrich and strengthen communities.
"We hope our support helps propel advances in neurodegenerative research," said Carol Ludwig, co-founder and president of the Carol and Gene Ludwig Family Foundation. "The outstanding work of Drs. Holtzman, Kipnis and Colonna, along with the depth of expertise at WashU Medicine, creates an extraordinary environment for advancing research and cultivating talent in this field."
About Washington University School of Medicine
WashU Medicine is a global leader in academic medicine, including biomedical research, patient care and educational programs with 2,900 faculty. Its National Institutes of Health (NIH) research funding portfolio is the second largest among U.S. medical schools and has grown 56% in the last seven years. Together with institutional investment, WashU Medicine commits well over $1 billion annually to basic and clinical research innovation and training. Its faculty practice is consistently within the top five in the country, with more than 1,900 faculty physicians practicing at 130 locations and who are also the medical staffs of Barnes-Jewish and St. Louis Children's hospitals of BJC HealthCare. WashU Medicine has a storied history in MD/PhD training, recently dedicated $100 million to scholarships and curriculum renewal for its medical students, and is home to top-notch training programs in every medical subspecialty as well as physical therapy, occupational therapy, and audiology and communications sciences.
Originally published on the WashU Medicine website






