This article highlights the work of advanced practice providers during National Advanced Providers Week, Sept. 26-30.
(SACRAMENTO)
The health care teams at UC Davis Health comprise a range of specialties and perspectives.
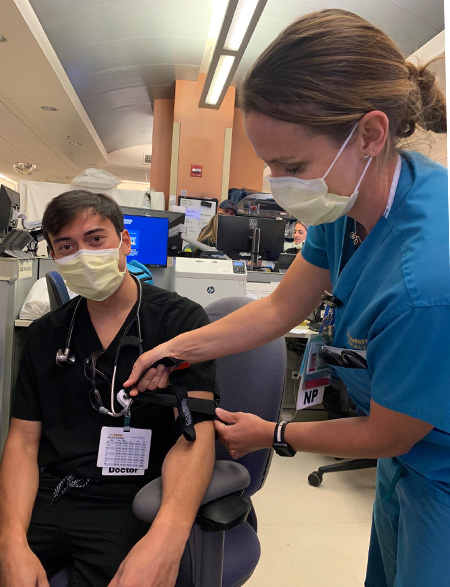
Among those experts are more than 350 advanced practice providers (APPs), including certified registered nurse anesthetists (CRNAs), nurse practitioners (N.P.s), physician assistants (P.A.s) and clinical nurse specialists (CNS). These clinicians work alongside the multidisciplinary teams to deliver exceptional care.
"These clinicians have gained advanced preparation for expanded clinical roles by earning a master's or doctorate degree and receiving dedicated training in a range of specialties," said Christi DeLemos, chief of advanced practice at UC Davis Medical Center. "Our CRNAs work with a team of anesthesiologists to deliver anesthesia and manage pain. Their team-based approach to anesthesia means better access to critical operative services needed at a level 1 trauma center."
Advanced practice nurses and clinical nurse specialists play a critical role in supporting evidence-based practice standards to shape organizational policy and health care team education. Their collective work has led to substantial improvements in diabetes care, the care of critically ill infants and children and adults with complex mental health and medical needs.
Half of the current APP staff members work in the health system's vast network of primary care and specialty clinics. This includes as neurology, trauma surgery, orthopedics, obstetrics, endocrinology, dermatology, infectious disease, palliative care and cardiology. Working alongside them are clinician educators from the Betty Irene Moore School of Nursing at UC Davis, who spend a majority of their time seeing patients and precepting students.

Increasing access and satisfaction
APP program leaders work to achieve two goals of the health system: increasing patient access and improving patient experience.
"Our physician colleagues have embraced APPs as a way to increase timely access to our specialty care clinics, many of which provide health care that is not available elsewhere in our region," said Aaron Wright, director for APPs based in UC Davis Health ambulatory clinics.
"When you think of a UC Davis Health N.P., it should remind you of a provider that listened, spent extra time to make sure you understood your diagnosis or treatment plan, and cared about your health outcomes," said Adebola Olarewaju, a pediatric N.P who works in the Department of Otolaryngology Head and Neck Surgery. "Having N.P.s as part of the team enhances the patient experience and supports continuity of care."
P.A. Keoki Leong loves working with people and learning how the team can best serve them.
"UC Davis Health is a stronger organization for having APPs because we bring such a depth of knowledge and unique experiences to the team," said Leong, who works on the Plastic and Reconstructive Surgery team. "We also help treat more patients and ease the load that our physician and resident colleagues go through from managing busy schedules."
The lure of the profession is growing. In fact, projections show that roughly two-thirds, or 67.3% of the workforce, will be APPs by 2030. This, at a time when a physician shortage between 40,000 and 105,000 is predicted in the same time frame.
"UC Davis Health's advanced practice providers are valuable members of our multidisciplinary care teams and are important partners in helping us increase access to patient-centered care across our service lines," said Susan Murin, interim dean of the UC Davis School of Medicine.
Setting new clinicians up for success
The Betty Irene Moore School of Nursing partners with the health system to offer two paths for new graduates to transition to practice.
The specialty track led by Danise Seaters, director of APP fellowship and education, offers eight specialty practice fellowships to support new graduate N.P.s and P.A.s in the critical first year as they transition into practice. The N.P. residency program is led by School of Nursing Interim Associate Dean for Practice Deb Bakerjian. It is designed to sharpen recent N.P. graduates' knowledge and skills in evidence-based primary care practice, critical thinking and independent decision making, as well as enhance their clinical teaching skills.
"By having our own programs, we are cultivating our own future APPs," Wright said.
"By leveraging our innovative educational programs and faculty expertise at the school of nursing and collaborating with our colleagues throughout UC Davis Health, we are becoming an indispensable partner to the clinical enterprise and providing tomorrow's health care, today," added Stephen Cavanagh, dean for the school of nursing.
Community service and growth
Beyond the clinical environment, UC Davis Health APPs work in the community. Currently a team of APPs from trauma surgery are leading an effort to teach the national course called 'Stop the Bleed' for 30 Sacramento-area schools.
"This effort will empower our community to make a life-or-death difference when a bleeding emergency happens," DeLemos said. "Team members have also organized a community fundraiser for a wraparound program supporting the long-term healing and recovery for violently injured youth, 13-to-26 years old, once they're back home in the community."
Currently, there are more than 80 open positions for APPs at UC Davis Health, which presents an opportunity for health care professionals and the patients they will serve.
"By January, I suspect we'll have well over 400 APPs to support the expansion of critical programs, improve access to care and patient experience," Wright explained.






