A new artificial intelligence-based system can accurately assess the chromosomal status of in vitro-fertilized (IVF) embryos using only time-lapse video images of the embryos and maternal age, according to a study from investigators at Weill Cornell Medicine.
AI-based tool can assist embryologists in determining both the embryo quality score and ploidy status, providing a comprehensive assessment of the embryo.
The new system, called "BELA," and described in a paper published Sept. 5 in Nature Communications, is the team's latest AI-based platform for assessing whether an embryo has a normal (euploid) or abnormal (aneuploid) number of chromosomes - a key determinant of IVF success.
Unlike prior AI-based approaches, BELA does not need to consider embryologists' subjective assessments of embryos. It thus offers an objective, generalizable measure and, if its utility is confirmed in clinical trials, could someday be used widely in embryology clinics to improve the efficiency of the IVF process.
"This is a fully automated and more objective approach compared to prior approaches, and the larger amount of image data it uses can generate greater predictive power," said study senior author Iman Hajirasouliha, associate professor of physiology and biophysics and a member of the Englander Institute for Precision Medicine at Weill Cornell Medicine.
The study's first author was Suraj Rajendran, a doctoral student in Hajirasouliha's laboratory. The embryology work for the study was headed by Nikica Zaninovic, associate professor of embryology in clinical obstetrics and gynecology and director of the Embryology Laboratory at the Ronald O. Perelman and Claudia Cohen Center for Reproductive Medicine (CRM) at Weill Cornell Medicine and NewYork-Presbyterian/Weill Cornell Medical Center. Dr. Zev Rosenwaks, director and physician-in-chief of the CRM and the Revlon Distinguished Professor of Reproductive Medicine in Obstetrics and Gynecology at Weill Cornell Medicine, co-authored the study.
Embryologists typically assess an IVF embryo's quality by examining it under a microscope. If it looks relatively normal but there are reasons to suspect possible problems, such as in cases of advanced maternal age, they may test its chromosomal status more directly. The "gold standard" test is a somewhat risky, biopsy-like procedure called preimplantation genetic testing for aneuploidy (PGT-A). In recent years, embryologists have been teaming up with computer/AI experts to find ways to automate some of this workflow and improve outcomes. In a 2022 study, Hajirasouliha and colleagues developed an AI-based system called STORK-A, which uses a single microscopic image of an embryo, plus maternal age and embryologists' scoring, to predict the embryo's ploidy status with about 70% accuracy.
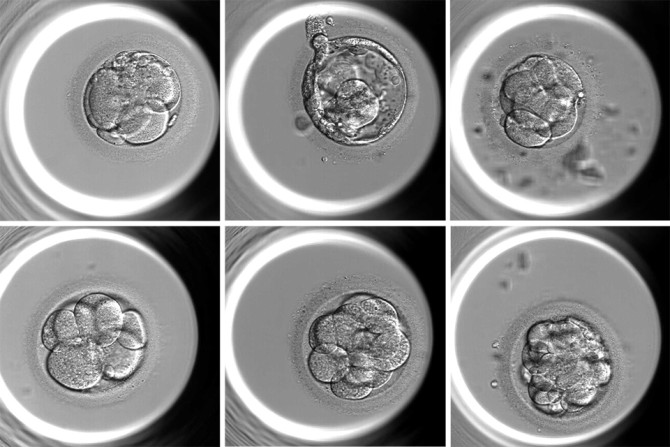
The researchers developed BELA to generate accurate ploidy prediction independently of embryologists' assessments. The heart of the system is a machine-learning model that analyzes nine time-lapse video images of an embryo under a microscope in a key interval about five days after fertilization to generate an embryo quality score. The system then uses this score and maternal age to predict euploidy or aneuploidy.
The researchers trained the model on a Weill Cornell Medicine CRM de-identified dataset with image sequences of nearly 2,000 embryos and their PGT-A-tested ploidy status. They then tested the model on new Weill Cornell Medicine CRM datasets and those from separate, large IVF clinics in Florida and Spain. They found that the model predicted ploidy status with moderately higher accuracy than previous versions and worked well for the external and internal datasets.
The next step, the researchers say, is to test BELA's predictive power prospectively in a randomized, controlled clinical trial, which they are currently planning.
"BELA and AI models like it could expand the availability of IVF to areas that don't have access to high-end IVF technology and PGT testing, improving equity in IVF care across the world," Zaninovic said.
The fact that BELA is set up to process a vast amount of image data for each embryo also suggests to the researchers that it could be used for more than ploidy prediction.
"Our hope is that this model could be useful also for general embryo quality estimation, prediction of the embryo development stage, and other functions that an embryology clinic could tailor for its own needs," Rajendran said.
Many Weill Cornell Medicine physicians and scientists maintain relationships and collaborate with external organizations to foster scientific innovation and provide expert guidance. The institution makes these disclosures public to ensure transparency. For this information, see profiles for Dr. Iman Hajirasouliha and Dr. Nikica Zaninovic.
Jim Schnabel is a freelance writer for Weill Cornell Medicine.