Madagascar is one of the last places where outbreaks of human bubonic plague still happen regularly.
Fleas carrying the plague bacterium Yersinia pestis can spread the disease through their bites. And while a species commonly known as "the rat flea" has been fingered as the main culprit in plague outbreaks, a species known as "the human flea" may play a secondary role.
As an investigator during plague outbreaks in rural Madagascar, medical entomologist Adelaide Miarinjara knew that many households were teeming with these human fleas. Miarinjara grew up in the island nation off the east coast of Africa and is now a postdoctoral fellow at Emory University, collaborating with the Pasteur Institute in Madagascar.
"We have observed huge variability in the number of fleas in different households in the same village," she says. "We might collect three or five fleas in one house and hundreds of them in another house."
Miarinjara led a study to solve the mystery of this variability.
PLoS Neglected Diseases published her team's findings: The abundance of human fleas is primarily associated with households that have a traditional dirt floor covered by a plant-fiber mat, as opposed to households with cement or board floors. A secondary risk factor was keeping animals in the house at night.
"Flea larvae need humidity, but not too much humidity, to survive," Miarinjara says, "so the dirt covered by the plant-fiber mat may be holding just the right amount of moisture for them to thrive."

A home in the Central Highlands of Madagascar. Residential structures vary greatly in rural areas, although homes typically consist of more than one level, with livestock often kept overnight in the bottom level.
She hopes that agencies seeking to improve people's lives in plague-endemic areas of Madagascar focus on upgrading the flooring in homes and constructing sheds separate from the households for animals.
"Flea infestation raises the risk for getting diseases and it has a big impact on the quality of life," Miarinjara says. "The constant bites are annoying and lead to lack of sleep."
Household flea infestations also promote the overuse of insecticides. Surveys by the researchers reveal that 80% of the households use insecticide to try to battle the fleas. Many people are buying liquid insecticides that are repackaged in empty plastic or glass containers, without labels or instructions for how to apply them, and sold in small, open-air markets.
Improper use of insecticides is a health risk to people who may be overexposed to the chemicals.
"Overuse of these chemicals is also dangerous because some fleas are developing resistance to insecticides — the frontline tools for battling plague outbreaks," Miarinjara says.
"Poverty related to housing construction is a primary challenge that this research identified," adds Thomas Gillespie, senior author of the study and professor and chair of Emory's Department of Environmental Sciences. "Resurfacing dirt floors in homes with concrete could improve a range of health and quality-of-life issues, from reducing flea populations in homes to making the floors easier to clean of contaminants such as fecal matter tracked in from the outside."
The Gillespie lab is a pioneer in the "one health" approach to epidemics — studying the interactions of people, domestic animals, wildlife and ecosystems to understand how germs jump across species.
The plague has afflicted humans at least as far back as the Bronze Age and has persisted through the centuries. The advent of antibiotics — which can effectively treat plague — turned the disease into a horror story from the past for much of the world.
In Madagascar, however, plague returns regularly to claim new victims. Cases typically originate in the rural rice-growing region of the central Highlands during the rainy season. Outbreaks there are associated with agriculture, deforestation, the black rat — and fleas.
Different flea species have evolved to prefer the blood of one animal over another, although they may feed on a variety of organisms if they are hungry enough.
Most plague research is centered on the rat flea, or Xenopsylla cheopis. Just one of its bites can transmit enough bacteria to infect someone with plague. In contrast, several bites from the human flea, Pulex irritans, are required to transmit the bacteria, making it a less potent spreader of plague but still a threat.
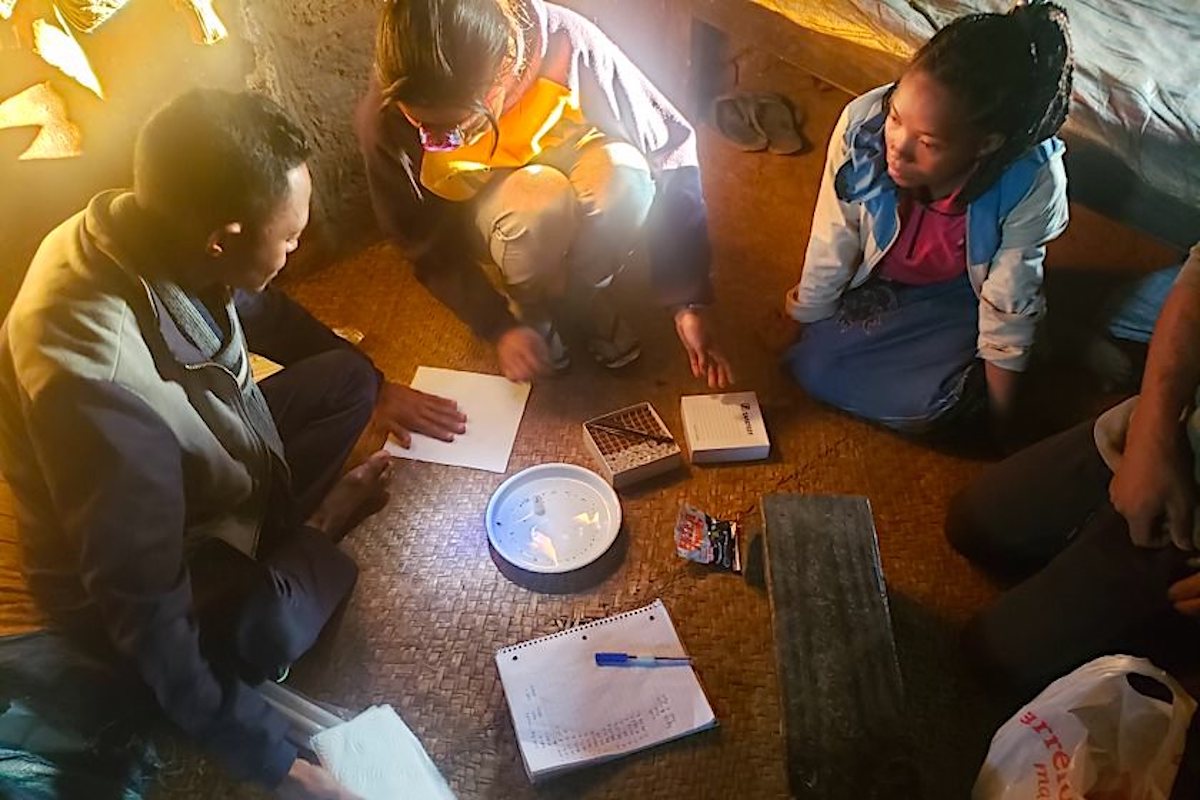
Researchers collect the fleas captured overnight in a candle trap while members of a household watch.
For the current paper, the researchers collected fleas from 126 households in four different villages. Rural Madagascar homes typically consist of more than one level. The bottom level is often used to keep livestock overnight and the second and third floors are where members of the family sleep, cook and eat.
The fleas were collected overnight on the second floor of the homes using simple traps — a lit candle set in a dish of soapy water. The fleas are attracted to the flickering light and drown when they hop into the dish.
The researchers painstakingly removed each drowned flea using tweezers, set them to dry on absorbent paper, and then transferred them to test tubes for laboratory identification and analyses.
The results showed that around 95% of the species collected in households were human fleas, mixed at times with a few rat fleas and a few from a third species that prefers to feed on cats and dogs. Collections were conducted in both the dry and rainy seasons with similar results.
"We're now looking deeper into what's going on with insecticide use in households," Miarinjara says. "We want to both sort out what is driving insecticide resistance among fleas and find ways to help people use insecticides safely and more effectively."
Co-authors of the current study include: Annick Reveloson, a PhD student at the University of Antananarivo in Madagascar; Stephen Mugel, an Emory PhD student set to graduate this May; Nick An, who graduated last year from Emory's BS/MPH program; Andry Andriamiadanarivo, a technician at Centre ValBio in Madagascar; and Minoarisoa Rajerison, Rindra Randremanana and Romain Girod, research scientists at the Pasteur Institute in Madagascar.
The research was funded by the Branco Weiss Society in Science Fellowship and the American Society of Tropical Medicine and Hygiene.
All photos by Adelaide Miarinjara.






