A better alternative for current incubator care: that's the goal of the interdisciplinary project in which PhD candidate Juliette van Haren developed prototypes for an innovative care environment. This new approach mimics the womb and may offer premature babies better development chances. On December 13th, she defeded her dissertation cum laude at the Department of Industrial Design.
Source: Cursor / Martina Silbrníková
The project, set up by doctors at Máxima Medical Centre (MMC), focuses on improving the care of premature babies. Thanks to a European subsidy, a collaboration was established between medical and technical disciplines.
Van Haren, with a background in both medical biology and industrial design, was ideally suited to tackle this challenge using design principles. "It's a very interdisciplinary project," she says. "I work closely with the Department of Biomedical Engineering (BME), which also leads the project."
No artificial womb
The idea is that the innovative care environment creates a safe and comfortable environment to optimally support the physical and mental development of premature babies. However, Van Haren emphasizes that the system is only intended for medical emergencies. "We deliberately aren't calling it an artificial womb," she explains. "That term suggests that it would completely take over the function of a real womb, which isn't the case."
The project inevitably raises ethical questions. That's why Van Haren believes it's important to clearly explain what the system does and doesn't aim to accomplish. "We focus exclusively on babies born between 24 and 28 weeks," she explains. In the Netherlands, the legal limit for intensive medical care for premature babies is 24 weeks, provided the child is viable.
Immersed in amniotic fluid
Despite advances in neonatal care, premature babies often suffer from long-term health problems, such as chronic lung diseases. That is why the consortium is working on a concept in which the baby remains immersed in an environment filled with amniotic fluid. This prevents the lungs from being directly exposed to air, allowing them to mature further.
"We can provide the child with oxygen and nutrients via the umbilical cord, which is connected to an artificial placenta after birth," Van Haren explains. "Medication can also be administered via this route, so we don't have to puncture the delicate skin."
"We cannot fully mimic the functions of the womb," she acknowledges. "But by creating an environment in which the baby is immersed in amniotic fluid, we may be able to offer many advantages. So it's not an artificial womb, but rather an amniotic fluid incubator."

Feedback loop
As this technology is still in its early stages of development, it cannot be applied to patients for now. In other countries, such innovations are often tested on animals, such as sheep. However, the consortium opted for an alternative approach to avoid animal testing as much as possible: testing using simulations.
Researchers from BME developed mathematical models for this purpose, a kind of digital twin of the cardiovascular system of a fetus, including the heart, blood vessels, and other relevant structures.
Industrial Design, in turn, designed physical patient simulators: lifelike dolls that mimic the physical structure and bodily functions of premature babies as much as possible. These physical models make it possible to perform tests under controlled conditions. By then linking the digital and physical models, crucial information can be exchanged.
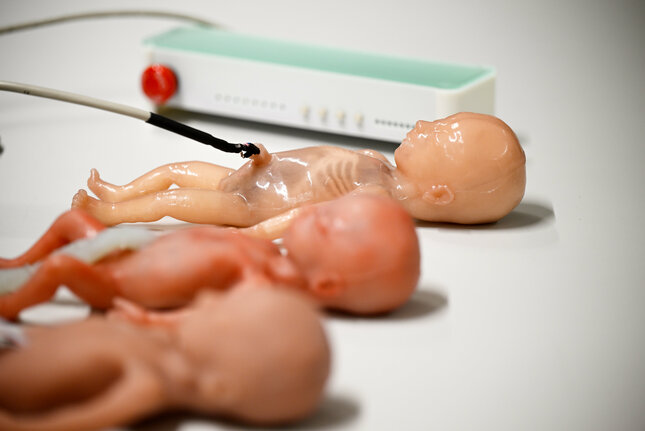
"For example, the physical simulators measure oxygen levels, after which the digital model calculates how these values affect blood pressure," Van Haren explains. "These calculations are then fed back to the physical models to refine the results. This creates a feedback loop that allows us to obtain increasingly accurate results."
Collaborative project
During the design process, feedback was collected from various stakeholders. For example, the prototypes were developed together with MMC doctors. "That collaboration was very valuable," says Van Haren. "It allows you to include the human dimension and make it truly tangible, which isn't possible with animal testing."
Students also played an important role in this collaborative project. "Many of the prototypes were co-developed by students," she continues. Not only did this result in valuable contributions, it also gave students the opportunity to gain practical experience within an interdisciplinary team.
Parent-child bonding
As the human aspect plays an essential role in the design, Van Haren worked closely with a patient organization consisting of parents of premature babies. "We believe the bond between the parents and the child is incredibly important," she emphasizes.
Although the amniotic fluid incubator offers protection, it can also form a barrier between parent and child. "We know that parent-child bonding is crucial for the well-being of both the baby and the parents," says Van Haren.
That's why a lot of thought was given to ways to strengthen that bond. One way to achieve this is through a 'womb phone' that parents could use to talk or sing to their baby. Another idea is the possibility of placing the incubator above the mother's belly for more physical proximity.
Perinate
For safe implementation, the technology needs to be thoroughly tested. One of the challenges is transferring a baby from the mother to the amniotic fluid incubator. "This has to happen quickly, because the oxygen supply stops as soon as the umbilical cord is cut," Van Haren explains. "The umbilical cord has to be connected to the artificial placenta immediately."
After birth, a fetus officially becomes a neonate, or newborn, which entails some biological changes. "However, our goal is to keep the baby in the fetal phase," says Van Haren. Some researchers even advocate a new term, such as 'fetonate' (a combination of fetus and neonate). Within the consortium, the term 'perinate' was retained, which refers to the transitional phase between a fetus and a newborn.
The project is part of a broader collaboration. For example, researchers from the University of Aachen are working on an artificial placenta and a technical prototype of the incubator, and colleagues in Milan are developing technologies for non-invasive monitoring.
Although the implementation of an amniotic fluid incubator will probably take years, Van Haren hopes that her research can make a valuable contribution. "Within the consortium we always say: we don't want to be the first; we want to do it right. In other words, first time right," she says.
"Now we at least have a physical setting in which we can brainstorm together and further develop the concept."






