A large research team led by nanotechnologist Roy van der Meel rebuild the body's own proteins and fats into nano delivery vans that get genetic medicines to exactly the right place in the body. In a joint effort with researchers from Radboudumc they worked for five years on this groundbreaking nanotransport system, the results of which were published in Nature Nanotechnology on 3 February 2025.
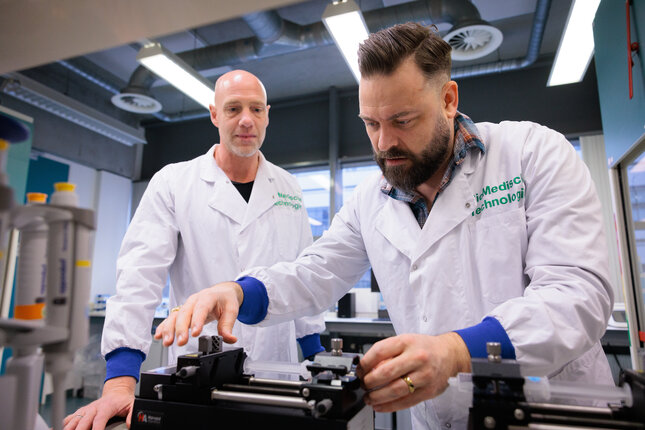
With his rugged beard and signature lumberjack blouse, nanotechnologist Roy van der Meel seems to have walked straight out of a Canadian forest hut instead of a high-tech lab. In Canada, Van der Meel did indeed work as a postdoc for Professor Pieter Cullis , founder of the nanotechnology used for messenger RNA vaccines. Five years ago, he exchanged Vancouver for a spot in Eindhoven. Professor Willem Mulder brought Van der Meel to TU/e because of his RNA nanotechnology expertise.
"My dream for the future is to develop nanotechnologies with our lab that will eventually end up in patients."
Roy van der Meer

Diseases that are currently difficult to cure, such as certain cancers and autoimmune diseases, can benefit from genetic drugs based on RNA. But then we must be able to get those medicines to the right place and that turns out to be a huge task.
"To address such a challenge, we need a top-notch team and access to both high-quality bioengineering and advanced preclinical models," says Mulder. "That's why we formed a research group with one foot in the Department of Internal Medicine at Radboudumc and the other - the Precision Medicine group - in the Department of Biomedical Engineering at TU/e."
Five years of construction
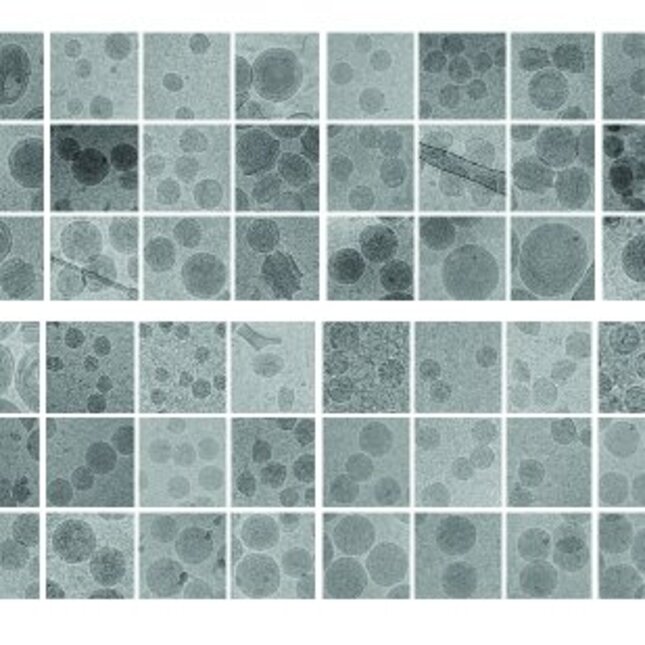
Over the past five years, Van der Meel has worked with a large team of researchers at TU/e and Radboudumc on new nanotechnology to get genetic drugs to the right place in the body. The publication of this nanotransport system (the aNP platform, ed.) in Nature Nanotechnology can rightly be called a breakthrough: the result of the vision that Mulder and Van der Meel set out in 2019 and the subsequent pioneering work.
Van der Meel: "I am extremely proud that we were able to start this work when our research group was still in its infancy. It required a lot of patience from the first three co-authors Stijn Hofstraat , Tom Anbergen , and Robby Zwolsman, with whom we worked intensively." The article is the starting signal for the development of immunotherapy for patients with the platform.
Body's own courier service
With the new nanotechnology, RNA drugs hitch a ride, as it were, on a transport system in your body: the body's own high-density lipoprotein (HDL) that transports cholesterol. Van der Meel likens himself to a courier for medicines. Van der Meel sees himself a bit as a courier of medicines: "When delivering packages, two things are important: that the contents of the package are well protected and that it arrives at the right place. Just like when delivering medicines into the body."
If you order something in a webshop, you can pack the package safely in styrofoam, but that is bad for the environment. That's why most packages these days are packed in cardboard and materials that you can recycle. Similarly, you can wrap medicines into more natural materials.
"Not that we make cardboard nanoparticles," Van der Meel jokes, "but particles from as many of the body's own materials as possible. There are synthetic components to build in the RNA in a stable way, but the main components of the aNP platform are the body's own fats and proteins." In this way, far fewer side effects are to be expected, and the 'delivery' is also more efficient.
The second step is the delivery itself. Van der Meel: "The standard route of the HDL parcel service is to the liver, where it neatly delivers the cholesterol packets collected in the body. By mixing HDL proteins with different fats, drugs can also be sent to immune cells or stem cells."
Immunotherapy based on genetic drugs
A disadvantage of existing medication is that it spreads throughout the body. "That's not a problem with paracetamol, which has few side effects, but it is with more intense drugs such as chemotherapy," says Van der Meel.
"Chemotherapy actually works very well but destroys all rapidly dividing cells. So not only cancer cells, but also healthy cells such as those in the intestines and hair follicles." This results in very unpleasant side effects for patients such as hair loss, intestinal problems, and a shortage of red blood cells, white blood cells, and platelets."
"Instead of throwing a big bowl of chemo into the body," says Van der Meel, "with many side effects as a result, there are many benefits to stimulating your own immune system to go after the cancer cells and clean them up."
"By delivering different RNA drugs to specific immune cells in the body using the aNP platform, we can control the immune system," says Van der Meel. "In the case of cancer or an infection, you want to stimulate the immune system to tackle diseased cells, while in the case of an autoimmune disease or after organ transplantation, the immune system needs to be curbed."
From lab to patient
And it does not stop at developing nanotechnology prototypes and proof-of-concept studies. In Canada, Van der Meel worked on the underlying nanotechnology and not on the resulting COVID mRNA vaccines. That is different now. The carefully constructed infrastructure that connects TU/e and Radboudumc ensures that innovations can be developed directly from lab to patient.
In addition to beautiful technology, the innovative research has also yielded a substantial patent portfolio. Mulder has therefore founded the biotech incubator BioTrip to further develop technologies into medicines with the help of drug developers and investors. TU/e and Radboudumc will also remain intensively involved in this.
Potential for personalised medicine
It is Van der Meel's dream to further develop aNP technology as a medicine, for example for types of cancer that are currently difficult to treat. "For example, it would be very interesting to use the aNP platform for chimeric antigen receptor T cell (CAR T) therapy, a relatively new cancer immunotherapy that is very effective. Precisely because this technology promises to offer a solution for cancer that is difficult to treat, which does not yet exist."

For this treatment, which currently easily costs hundreds of thousands of euros, immune cells (T cells) are taken from patients, then genetically modified in the lab so that they can recognize and eliminate cancer cells and then returned to the patient. It is precisely because each patient is made in the lab (ex vivo) that the treatment is so expensive.
Van der Meel: "With our aNP technology, it is theoretically possible to develop these personal medicines, by administering our nanoparticles directly to the patient (in vivo). They can then achieve the same as a CAR T treatment in cooperation with their own immune system, but with cells that are already in your body."
"This so-called in vivo CAR immunotherapy has many potential advantages: it takes much less time, is much cheaper, and can be made suitable for multiple types of cancer. Although this is already being tested on a small scale in patients, this application is still in its infancy", Van der Meel emphasizes.
The 'Wies Alliance'
Although the technology described in the current Nature Nanotechnology publication is very promising, it may take years before a working drug is on the market. In the meantime, people die of forms of cancer that are difficult to treat, something that suddenly came close to home for Mulder and Van der Meel when colleague Paul Janssen lost his son Wies to incurable brain stem cancer.
"There is actually no treatment for that at all, because it is very difficult or often not possible at all to get into the brain stem surgically or with medication," says Van der Meel. "It would be great if we had a solution."
"I believe in the potential of our nanotechnology to stimulate immune cells that then go after brain tumour cells. And I'm not saying that it is guaranteed to work," warns Van der Meel. "But we are working on that. We'll try."
Janssen put his son's treating physician Dannis van Vuurden in touch with the Precision Medicine group in Eindhoven and immunologist Mihai Netea at Radboudumc. There is now a collaboration between TU/e, Radboudumc, and the Princess Máxima Center in the ' Wies Alliance ' to develop better treatments for brain stem cancer.
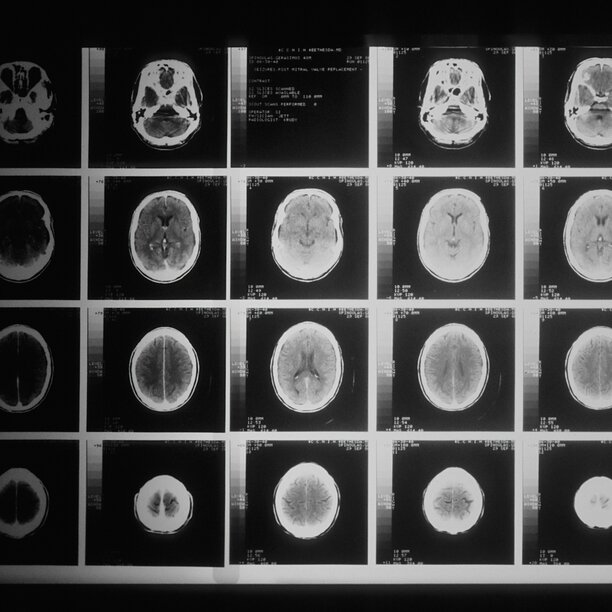
The Wies Alliance
The Wies Alliance is a partnership between the Princess Máxima Center, Eindhoven University of Technology (TU/e) and Radboudumc, founded in memory of Wies, who died at a young age in 2020 from brain stem cancer (DIPG). The aim of this alliance is to promote research into new treatments for brain stem cancer in children, with a focus on immunotherapy.
Future dreams
When asked about the future possibilities of RNA therapies, Van der Meel dares to dream out loud. "RNA drugs make it possible to develop very precise personalised medicines in a short period of time. Think of cancer vaccines, immunotherapies that are developed based on the genetic code of individual cancer patients. But also the possibility of curing very rare diseases with the help of gene editing.
"I am very proud of this publication in Nature Nanotechnology," concludes Van der Meel, "but my dream for the future is to develop nanotechnologies with our lab that will eventually end up in patients, and not just in publications. And of course that doesn't work with engineers alone, because a lot of knowledge from all kinds of fields is needed here."
The collaboration of experts from different disciplines is therefore also characteristic of the Precision Medicine group. Mulder and Van der Meel: "In our group, we train super experts, who we have work together on bigger stories. We believe that the aNP technology is a game changer and firmly believe that it will enable the development of true immunotherapies for patients in the future."






