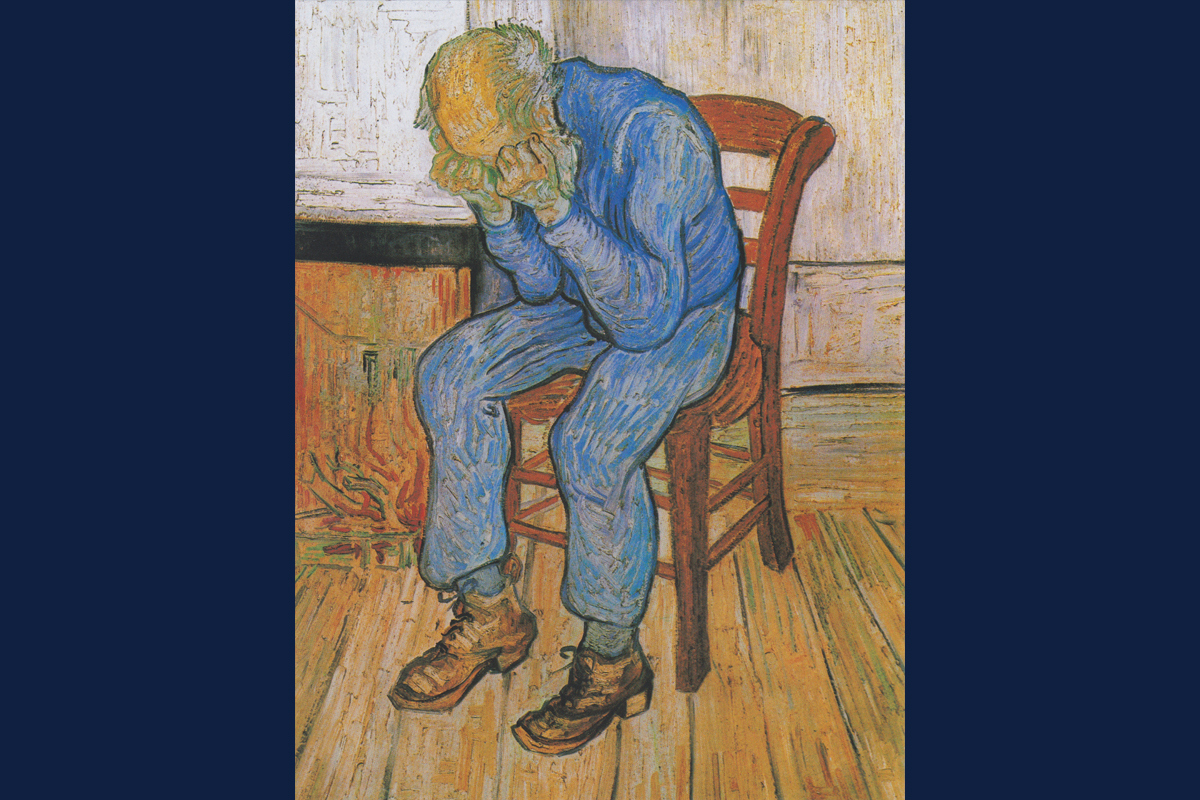
Treatments modulating the neurotransmitter GABA and its main receptors in the brain could help address both the affective and cognitive symptoms associated with depression, such artist Vincent Van Gogh is suspected to have experienced, the authors of a new paper say.
"Sorrowing Old Man (At Eternity's Gate)," Vincent van Gogh, Public domain, via Wikimedia Commons
CHAMPAIGN, Ill. - Depression is a complex condition correlated with multiple differences in brain function and mechanisms. A new paper spanning known data about the neurotransmitter GABA and its principal receptors showcases evidence of the receptors' importance in depression and potential as therapeutic targets.
Based on evidence from research on the receptors' function in the brain and the drugs that can activate or inhibit them, the authors propose possible mechanisms by which GABA-modulating treatments could help address the cognitive and affective symptoms associated with depression.
Authors Bernhard Luscher of Penn State University, Jamie Maguire of Tufts University, Uwe Rudolph of the University of Illinois Urbana-Champaign and Etienne Sibille of the University of Toronto and the Centre for Addiction and Mental Health published their paper in the journal Trends in Pharmacological Sciences.
Most currently available antidepressant drugs are designed to increase the function of the neurotransmitter serotonin, said Rudolph, a professor of comparative biosciences at Illinois. However, over the past two decades or so, research has shown depression and its symptoms to be complex, with the neurotransmitter GABA and its main receptor, GABA-A, playing an important, though not well understood, role.
"Defects in the function of GABA and its principal receptors have long been suspected of contributing to depressive disorders," said Luscher, a professor of biology, biochemistry and molecular biology, and psychiatry at Penn State. His group first found compelling evidence of a causal link between depression and GABA functional defects in a 2010 study of mice.
"The notion that GABA and GABA-A receptor functional defects are at the core of depressive disorder was vindicated in 2019 when the FDA approved Brexanolone as a first treatment for peripartum depression, and even more so through recent clinical trials which demonstrate that very similar compounds are also effective in more common variants of Major Depressive Disorder. Brexanolone is a synthetic version of a natural hormone that is known to act mainly by increasing the function of GABA at GABA-A receptors," Luscher said.
GABA is the most prominent inhibitory neurotransmitter in the brain, helping the brain to keep balance and regulate signals between neurons.
"Like with your car, you need the gas pedal and you need the brake. And not only that, you have to maintain the balance," Rudolph said.
Neurosteroids act as positive modulators of GABA-A receptors. Chronic stress - a major risk factor for depression - decreases neurosteroid signaling, impairing the inhibitory balance, said Maguire, a professor of neuroscience at the Tufts University School of Medicine. Conversely, enhancing neurosteroid signaling enhances GABA signaling and improves behavioral outcomes - evidence that neurosteroids regulate mood through their action on GABA-A receptors.
"These studies implicate impaired neurosteroid signaling in depression and suggest that treatments stimulating GABA-A receptors may exert their antidepressant effects by targeting this underlying neurobiological mechanism," Maguire said.
One of the more confusing points to emerge in preclinical studies is that both drugs that boost GABA-A receptor activity and those that suppress it may have antidepressant effects. In the new paper, the authors propose for the first time mechanisms that explain how both gradually boosting the function of GABA-A receptors and acutely and transiently inhibiting them can alleviate symptoms.
Compounds that promote GABA-A receptor activity - and consequentially, dampening activity in neurons - can help to treat depressive symptoms based on GABA deficits or too much activity, such as in states of aging or chronic stress, the authors say. Conversely, those that inhibit GABA-A, and thus allow more activity between neurons, can help other pathways in the brain rapidly "reset" from a stressed or depressed state.
The paper also makes a case for GABA-A receptors as a target to treat the cognitive impairment often correlated with depression, but not alleviated by treatments that focus on serotonin or other neurotransmitters. Research from Sibille's lab on the role of GABAergic deficits has found links to cognitive deficits, not only in depression but in conditions like Alzheimer's disease as well.
"We have uncovered the changes in the human postmortem brain, and then showed causality using genetic and environmental manipulations in rodent models," Sibille said. "These studies have led to the foundation of a biopharmaceutical company, DAMONA Pharmaceuticals, dedicated to the pioneering treatment of cognitive deficits across brain disorders, including depression and Alzheimer's disease."
Taken together, the available data on GABA-A receptors, their function in the brain, the brain's response to a lack of GABA activity, and the success of a GABA-A-promoting drug to treat peripartum depression point to GABA-A receptors as an important element in depression and crucial target to consider for treating not only the affective symptoms but also cognitive ones, the authors conclude.






