Mescaline, a natural hallucinogen known since ancient times, was not only a favorite of artists and bohemians but also a mainstay of brain research throughout the first half of the 20th century, until it was eclipsed in the 1950s by the much more potent, synthetic LSD. Now, with the resurgence of interest in psychedelics as potential therapies for psychiatric disorders, mescaline research is again raising hope for treatment. Unfortunately, reawakened attention is pushing its natural source, the small, slow-growing peyote cactus, to the brink of extinction. In a new study, Weizmann Institute of Science researchers have made the first, crucial move toward ensuring sustainable production of mescaline: They have revealed, step by step, how exactly it is manufactured in peyote.

"Learning how to copy this natural process with biotechnology will help ensure a steady supply of mescaline for the development of new psychiatric drugs," says Dr. Shirley (Paula) Berman, who led this research in Prof. Asaph Aharoni's lab in Weizmann's Plant and Environmental Sciences Department.
Scientists are still not sure why a select few cacti produce mescaline. Possibly, it protects the bulbous, ground-hugging peyote, which has no spines, by imparting a bitter taste to its flesh or deterring insects and other predators from consuming the cactus by altering their physiological state. In that case, however, why does the towering San Pedro cactus, a distant relative of peyote that does have spines, also produce mescaline, though in smaller amounts?
The biochemical pathway of mescaline manufacture has been studied for years, but most of the steps remained hypothetical, and the enzymes involved in each step were unknown.
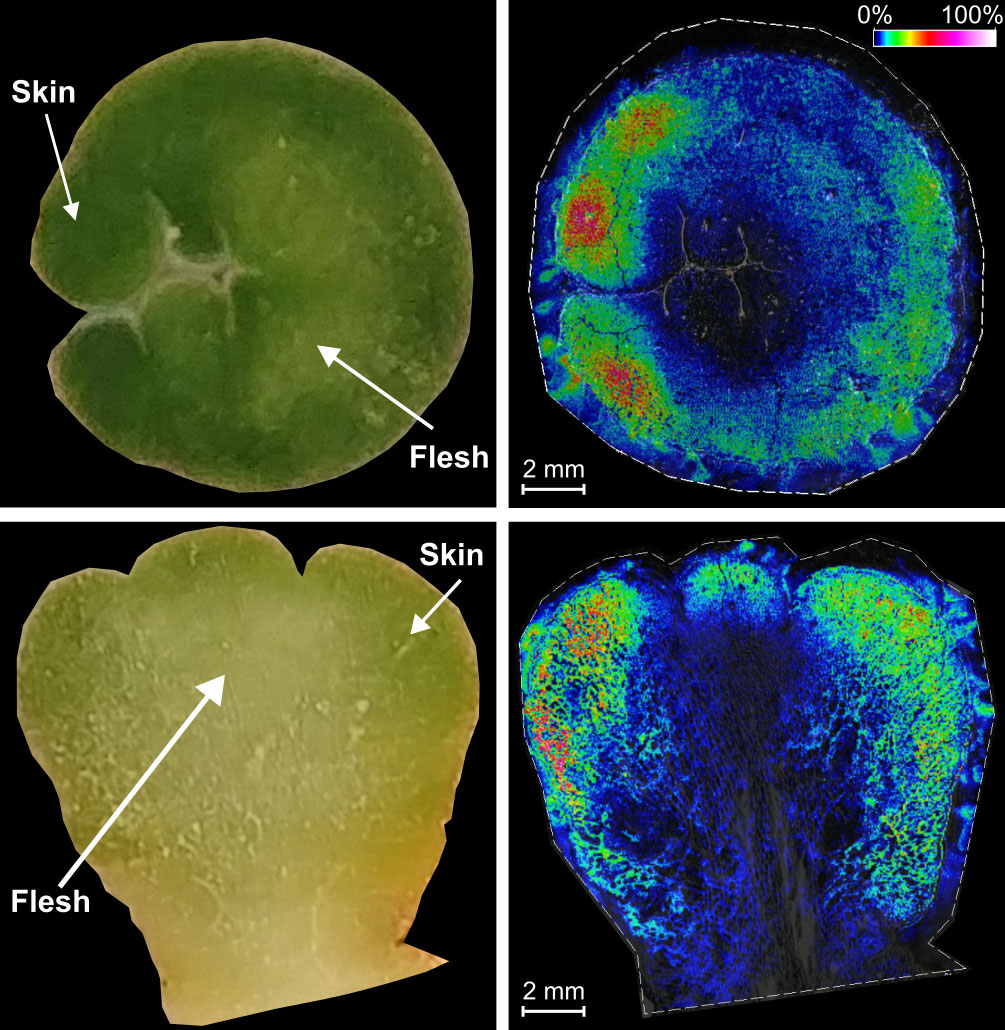
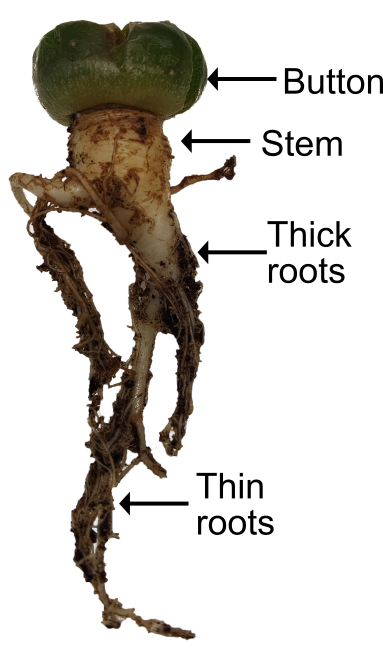
In the new study, Berman and colleagues started out by deciphering the entire genome of the peyote cactus, determining which genes are expressed in which parts of the plant, particularly in the outer layers of its crown, called the button, where the highest concentration of mescaline was measured. Using mass spectroscopy, they then identified a series of candidate molecules that were possibly involved in mescaline production. They also selected candidate genes for each type of enzyme having the potential for catalyzing the relevant biochemical reactions and tested their activities after expressing each gene in bacteria, yeast or model plants. With this knowledge in hand, they completed the puzzle by reconstructing the entire pathway of mescaline manufacture in peyote.
""Mescaline interacts with receptors for the brain chemical serotonin, which serves as the target for an entire group of drugs against depression, OCD and other mood-related disorders"
Starting with one amino acid - tyrosine - mescaline generation proceeds in six steps that involve four families of enzymes and three types of biochemical reactions. The researchers documented all of these, down to the minutest detail, even determining how very similar enzymes might help produce different plant chemicals from a particular molecule, depending on the way this molecule docks within each enzyme's 3D structure. Throughout the study, they compared mescaline manufacture in peyote to the significantly different way in which it is made in the San Pedro cactus, gaining more insights into the biology of both.

Finally, the scientists set out to reconstruct the pathway outside of the cacti, and they managed to recreate five of the six mescaline manufacture steps, including the generation of all the intermediate molecules, in a model tobacco plant. The task was challenging because the plant kept hijacking some of these intermediates for processes unrelated to mescaline. This led the researchers to conclusions as to which intermediates would need to be produced in larger amounts in an artificially engineered pathway in order to arrive at the desired result.
"In future studies, we hope to reproduce the entire pathway in the lab, so as to develop a method for manufacturing useful quantities of natural mescaline in yeast or in plants that are larger and faster-growing than peyote," Berman says. She adds that the peyote population is dwindling in nature, partly because of unsustainable harvesting by peyote hunters who cut the plant too close to the root. Creating alternative sources of natural mescaline could help preserve the endangered cactus while ensuring a supply of mescaline for permitted uses. Though it is banned in many countries, its use is usually allowed in religious ceremonies and, with special permission, in scientific and medical research.
"Mescaline interacts with receptors for the brain chemical serotonin, which serves as the target for an entire group of drugs against depression, OCD and other mood-related disorders," Berman explains. "Next-generation drugs that will be developed on the basis of mescaline and other psychedelics might be longer-lasting and have fewer side effects than the existing ones."
In addition to making mescaline available for drug discovery, causing plants other than peyote to make mescaline will also enable studies clarifying the hallucinogen's functions in the cacti. Says Berman: "We can only guess what these functions could be, but we'll know what they are if we see, for example, that insects avoid a plant engineered to produce large quantities of mescaline, or that this plant is unusually resistant to UV radiation."
Science Numbers
LSD is 1,000 to 3,000 times more potent than mescaline, and mushroom-derived psilocybin is 30 times more potent than mescaline, but the effects of mescaline last longer - about 11 hours - compared to about 8 hours for LSD and close to 5 hours for psilocybin.
It takes about 6 peyote buttons to extract enough mescaline for a mood-altering "high."
Peyote makes 3 times more mescaline per gram of cactus flesh than the San Pedro cactus does.
Also participating in the study were Dr. Luis Alejandro de Haro, Dr. Ana-Rita Cavaco, Dr. Sayantan Panda, Dr. Gabriel Lichtenstein, Hila Harat, Dr. Adam Jozwiak, Dr. Jianghua Cai, Dr. Sagit Meir and Dr. Ilana Rogachev of the Plant and Environmental Sciences Department; Drs. Younghui Dong, Yoav Peleg and Uwe Heinig of the Life Sciences Core Facilities Department; and Dr. Nikolay Kuzmich of the Nancy and Stephen Grand Israel National Center for Personalized Medicine.
Prof. Asaph Aharoni is head of the Harry and Jeanette Weinberg Center for Plant Molecular Genetics Research, of the Melvyn A. Dobrin Center for Nutrition and Plant Research, and of the Charles W. & Tillie K. Lubin Center for Plant Biotechnology. His research is supported by the Laura Gurwin Flug Family Fund; the Wolfson Family Charitable Trust & Wolfson Foundation; and by Monica Armour. He is the incumbent of the Peter J. Cohn Professorial Chair.






