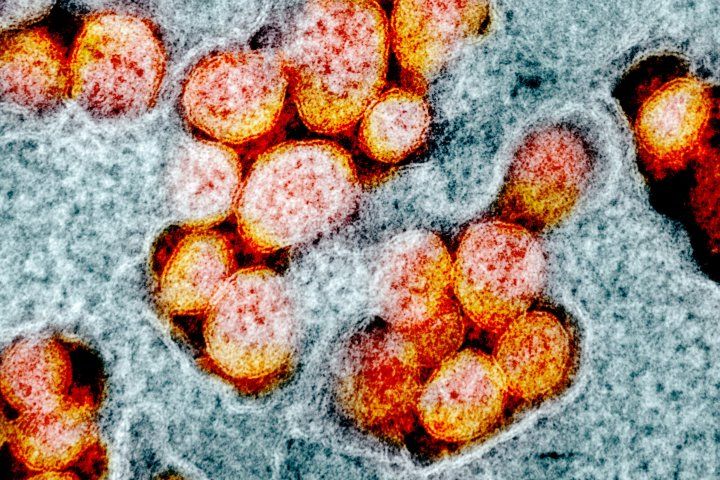
Plitidepsin was 27.5-fold more potent against SARS-CoV-2 than remdesivir, a drug that received FDA emergency use authorization in 2020 for the treatment of COVID-19, according to new research. Image by NIH
Scientists at UC San Francisco's Quantitative Bioscience Institute (QBI) and the Icahn School of Medicine at Mt. Sinai (ISMMS) in New York have shown that plitidepsin (Aplidin), a drug approved by the Australian Regulatory Agency for the treatment of multiple myeloma, has potent antiviral activity against SARS-CoV-2, the virus that causes COVID-19.
In laboratory experiments reported in Science on Jan. 25, plitidepsin, a compound originally discovered in a Mediterranean sea squirt, was 27.5-fold more potent against SARS-CoV-2 than remdesivir, a drug that received FDA emergency use authorization in 2020 for the treatment of COVID-19. In addition, in two preclinical models of COVID-19, plitidepsin showed a 100-fold reduction in viral replication in the lungs and demonstrated an ability to reduce lung inflammation.
The studies were led by the laboratories of Nevan Krogan, PhD, director of the QBI, part of the UCSF School of Pharmacy, and Adolfo García-Sastre, PhD, professor of microbiology and director of the Global Health and Emerging Pathogens Institute at ISMMS.
In 2020, in response to the COVID-19 pandemic, Krogan, also a senior investigator at Gladstone Institutes, brought many UCSF labs together in the QBI Coronavirus Research Consortium (QCRG), which played a major role in the new research.
In a separate publication posted to the bioRxiv preprint server, the UCSF and ISMMS researchers, in collaboration with Greg Towers, PhD, and Clare Jolly, PhD, of University College London, show that plitidepsin has antiviral activity against the recently identified B.1.1.7 variant of SARS-CoV-2 which is comparable to the drug's activity against the original SARS-CoV-2 strain. Additionally, they found plitidepsin to be about 100 times more potent than remdesivir in human epithelial cells.

Nevan Krogan, PhD
"From the start, our scientific investigations with the QCRG were to research where and how the SARS-CoV-2 virus was co-opting its human host to thrive, survive and become deadly," said Krogan. "That research led us to a biologic pathway, the eukaryotic translation machinery, where inhibition of the pathway showed significant antiviral activity in cell culture. One of the promising agents that arose from our screen of drugs that inhibit this pathway was plitidepsin. Our preclinical data showing increased potency compared to remdesivir, and in conjunction with recent early clinical data showing promise in COVID-19 patients, as reported by the drug's manufacturer, suggest plitidepsin should be further evaluated as a COVID-19 therapy."
García-Sastre said, "The ongoing COVID-19 pandemic has created an immediate need for antiviral therapeutics that can be moved into the clinic urgently. This led us to screen clinically approved drugs with established safety profiles. Our previous study of the SARS-CoV-2's interactions with human host cells led us to a protein known as eEF1A, which is involved in translating mRNA into proteins, as a potential druggable target to inhibit SARS-CoV-2 replication."
The studies were conducted in close collaboration with PharmaMar, a Spanish pharmaceutical company that first isolated plitidepsin (trade name Aplidin) from a sea organism known as Aplidium albicans.
"Plitidepsin is an extremely potent inhibitor of SARS-CoV-2, but its most important strength is that it targets a host protein rather than a viral protein," said Kris White, PhD, assistant professor of microbiology at ISMMS, first author of the Science paper. "This means that if plitidepsin is successful in the treatment of COVID-19, the SARS-CoV-2 virus will be unable to gain resistance against it through mutation, which is a major concern with the spread of the new U.K. and South African variants."
Krogan said the work is further validation of the QCRG's focus on host proteins as a strategy to fight COVID-19 and other viral diseases.
"It is host mechanisms that permit the SART-CoV-2 virus to wreak havoc," Krogan said. "By targeting host factors that enable or facilitate disease, we have the potential to have a more far-reaching impact in drug development. In this case, SARS-CoV-2 and its mutant strains, and possibly other viruses that leverage the same pathway, may also be susceptible to the same therapeutic agents that inhibit this virus-host interaction."
Authorship and funding: This work was funded by grants from the National Institute of Mental Health and the National Institute of Allergy and Infectious Diseases (NIAID), both part of the National Institutes of Health; the Defense Advanced Research Projects Agency; the Center for Research for Influenza Pathogenesis; the Centers of Excellence for Influenza Research and Surveillance of the NIAID; the Centers of Excellence for Integrative Biology of Emerging Infectious Diseases of the Agence Nationale de la Recherche (France); F. Hoffmann-LaRoche AG; Vir Biotechnology, Centre for Integrative Biological Signalling Studies (CIBSS), European Research Council (ERC) and QCRG philanthropic donors. Co-author Kevan Shokat is a Howard Hughes Medical Institute investigator. A complete list of authors and full funding information is available in the Science paper.






