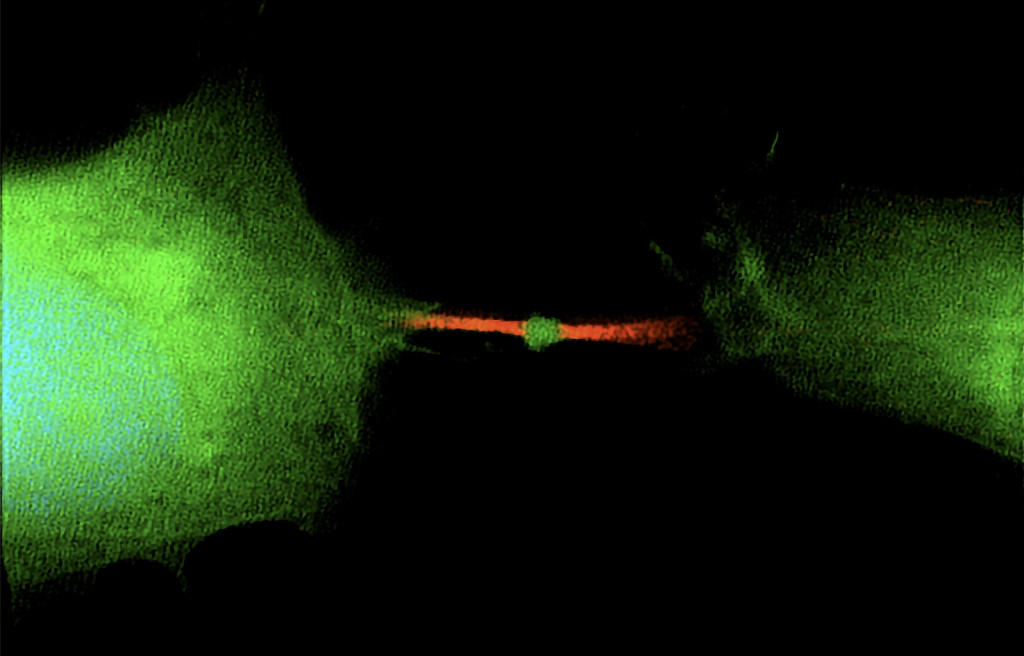
RNA translation marked by bright green reveals two soon-to-be-separate human cells still connected by the red microtubules that provide some structure during cell division. The dot of green in the middle is a midbody, a structure that will be released when division is complete and free to carry its significant genetic cargo away to other cells. Skop Lab
Once thought to be the trash can of the cell, a little bubble of cellular stuff called the midbody remnant is actually packing working genetic material with the power to change the fate of other cells - including turning them into cancer.
It's a surprise to many people, according to Ahna Skop, a University of Wisconsin-Madison genetics professor, that when one cell divides into two, a process called mitosis, the result is not just the two daughter cells.

Ahna Skop, a UW-Madison genetics professor, whose lab led the study.
"One cell divides into three things: two cells and one midbody remnant, a new signaling organelle," says Skop. "What surprised us is that the midbody is full of genetic information, RNA, that doesn't have much to do with cell division at all, but likely functions in cell communication."
In a study published today in the journal Developmental Cell, Skop's lab and collaborators from the Pasteur Institute in Paris, Harvard Medical School, Boston University and the University of Utah analyzed the contents of midbodies - which form between the daughter cells during division - and tracked the interactions of the midbody remnants set free after cell division. Their results point to the midbody as a vehicle for the spread of cancer throughout the body.
"People thought the midbody was a place where things died or were recycled after cell division," Skop says. "But one person's trash is another person's treasure. A midbody is a little packet of information cells use to communicate."
The midbody's involvement in cell signaling and stimulating cell proliferation has been investigated before, but Skop and her collaborators wanted to look inside the midbody remnants to learn more.

Sungjin Park, a senior scientist in Skop's lab, is the lead author of the new study.
What the researchers found inside midbodies was RNA - which is a kind of working copy of DNA used to produce the proteins that make things happen in cells - and the cellular machinery necessary to turn that RNA into proteins. The RNA in midbodies tends to be blueprints not for the cell division process but for proteins involved in activities that steer a cell's purpose, including pluripotency (the ability to develop into any of the body's many different types of cells) and oncogenesis (the formation of cancerous tumors).
"A midbody remnant is very small. It's a micron in size, a millionth of a meter," Skop says. "But it's like a little lunar lander. It's got everything it needs to sustain that working information from the dividing cell. And it can drift away from the site of mitosis, get into your bloodstream and land on another cell far away."
Many midbody remnants are reabsorbed by one of the daughter cells that shed them, but those that touch down on a distant surface, like a lunar lander, may instead be absorbed by a third cell. If that cell swallows the midbody, it may mistakenly begin using the enclosed RNA as if it were its own blueprints.
Previous research showed that cancer cells are more likely than stem cells to have ingested a midbody and its potentially fate-altering cargo. Stem cells, which give rise to new cells and are valuable for their pluripotency, spit a lot of midbodies back out, perhaps to maintain their pluripotency.
Future research may be able to harness the power of midbody RNA to deliver drugs to cancer cells or to keep them from dividing.
"We think our findings represent a huge target for cancer detection and therapeutics," says Skop, whose work is supported by the National Institutes of Health.
The researchers identified a gene, called Arc, that is key to loading the midbody and midbody remnant with RNA. Taken up long ago from an ancient virus, Arc also plays a role in the way brain cells make memories.
"Loss of Arc leads to the loss of RNA in the midbody and a loss of the RNA information from getting to recipient cells," Skop says. "We believe this memory gene is important for all cells to communicate RNA information."
Sungjin Park, a senior scientist in Skop's lab, is the lead author of the new study. Skop and collaborators also have a patent pending on two new methods that make it easier to isolate midbody structures from cell media or blood serum, improving cancer diagnostics.
This research was funded in part by grants from the National Institutes of Health (R01 GM139695-01A1, R01 NS115716, and R01 GM122893 and GM144352) and the French Fondation ARC for cancer research.






