Community leaders from across the UK joined arms with public health experts to brainstorm ways to help plug the gap in health inequalities.

Organised by the Department of Population Health Sciences, dozens of community figures who work with youths, families, and under-represented communities from Lambeth, Bradford and Kent met up with researchers and public health officials to highlight health inequalities in the community and figure out practical ways alleviate these.
Multisectoral collaborations are critical for addressing the intersections of social determinants that drive health inequalities. We don't know enough about how best to build equitable and sustainable partnerships across health and non-health sectors. We brought together stakeholders from communities, charities, local public health, and industry to discuss who should be involved, realistic priorities, and pathways to sustainability."
Seeromanie Harding, Professor of Social Epidemiology
The goal of the day was to brainstorm practical steps to move towards a Multisectoral Collaborative, which describes a group formed to promote inclusion, diversity and equity in research to work towards health equity. Participants were invited to develop this concept and identify specific ways they could work together to create something realistic, sustainable and mutually beneficial.
The workshop took place at the Marylebone headquarters of property development company Delancey, who are an industry partner of the initiative. The day took on a 'World Café' structure, which is a widely used research method that sparks collaborative conversations and collective intelligence on a topic. A live scribe was present throughout the day, creating illustrations based on the conversations that were taking to engage audiences and drive change through visual storytelling.
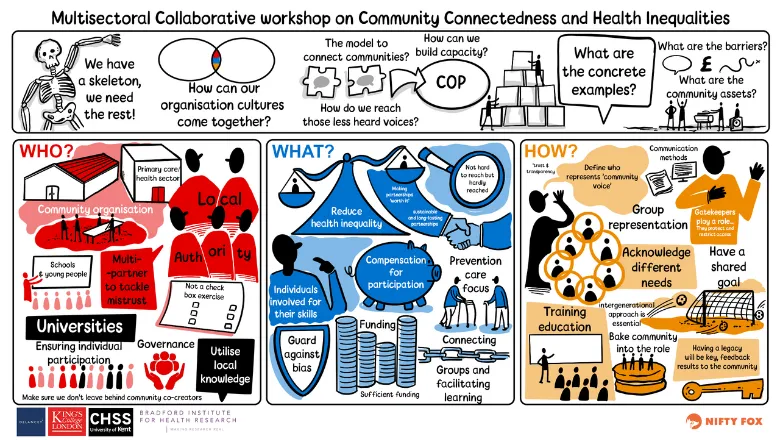
Participants from initiatives such as Lambeth HEART, Citizen Science and Faith in Communities were tasked with answering three prompts for the morning discussion. These included: 'What are the actionable priorities for a UK-wide multisectoral collaborative?'; 'Who should be part of such a collaborative and why?'; and 'How can community voices be embedded in this collaborative?'
Some of the areas highlighted by participants in response to these prompts included the importance of building trust between researchers, community organisations and community members.
Communication was also emphasised, with sensitivity around language barriers and the importance of using clear and accessible communication to ensure a two-way dialogue. Capacity building was also highlighted, with importance placed on training community members in research skills and data use to influence decision making for funding.
We had an amazing day full of enthusiastic, productive and honest conversations. Stakeholders shared their understandings of problems and solutions, with an emphasis on prevention of diseases and sustainability of partnerships. They discussed pathways for inclusive leadership, shared leadership and governance, and for shared capacities and resources.
Professor Harding
She added: "Some cross cutting themes related to the importance of integrating intergenerational connectedness and of promoting a shift in thinking away from 'hard to reach' to 'hardly reached' communities. We will continue to develop these ideas as we seek opportunities for multisectoral partnerships for tackling health inequalities locally, nationally and internationally."
The project, titled 'Multisectoral collaboratives, community connectedness and health inequalities', was a collaborative initiative led by researchers from King's, the University of Kent and the Bradford Institute for Health Research.

The term 'health inequalities' describes unfair and avoidable differences in health across the population and between different groups within society. These include how long people are likely to live, the health conditions they may experience and the care that is available to them. Health inequalities can involve differences:
- Health status (for example, life expectancy)
- Access to care (for example, availability of given services)
- Behavioural risks to health (for example, smoking rates)
- Wider determinants of health (for example, quality of housing)






