Black youth, males and obese patients among those at higher odds of severe disease
When Blake Martin, MD, packs up his two tots for preschool and outings, he knows their chances of ending up in the hospital with COVID-19 are slim. Many parents breathed huge sighs of relief when the mysterious virus of 2020 turned its focus away from the country's littlest citizens.
Yet symptom checks and fitted masks remained part of the Martin family routine, not just because his 1- and 3-year-old could end up being outliers - like the pediatrician's own severely sick patients struggling in hospital beds. But also because of the critical care doctor's desire to protect all children.
Now Martin, the lead author of a recently published study, hopes the research looking at factors behind the most severe pediatric cases helps sway more parents to do the same.
Top risk factors: being Black, male or obese
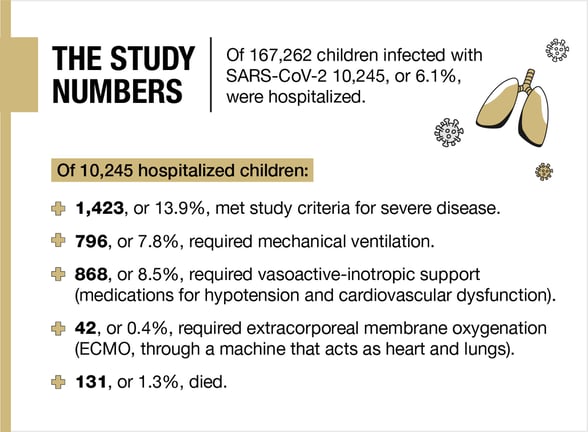
Researchers scoured records of over 10,000 children who ended up hospitalized with COVID-19, checking race, age, sex, comorbidities, weight, vital signs and lab values in search of correlations.
 In one of the largest pediatric-focused studies so far, the analysis involved 56 sites, over 1 million records, and more than 167,000 SARS-CoV-2-positive youth 18 and younger.
In one of the largest pediatric-focused studies so far, the analysis involved 56 sites, over 1 million records, and more than 167,000 SARS-CoV-2-positive youth 18 and younger.
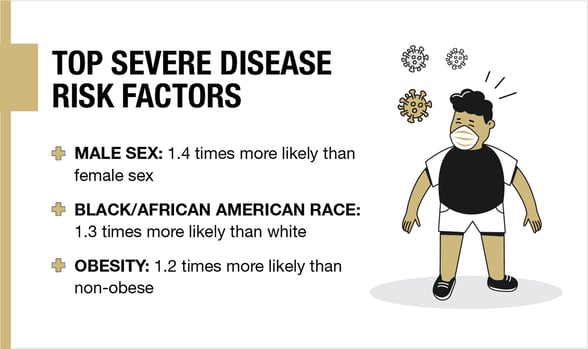
The top individual predictors of severe disease were being male, Black, obese and having a pediatric complex chronic condition (PCCC). PCCC categories include (among others) cancer and cardiovascular- and respiratory-related diseases.
"While the study confirms that, overall, kids do very well, there are groups of children who are at risk of getting really sick and even dying," said Martin, assistant professor of pediatrics at the University of Colorado School of Medicine and pediatric intensivist at Children's Hospital Colorado, one of the study's sites."
"So even if we personally aren't going to be affected by one of these severe cases, we (or our kids) probably know somebody who could."
Prime implication: raising a red flag
The study was one of the first to look at highly detailed data in youth, including vital signs and lab results throughout each child's hospitalization. What scientists discovered could accelerate treatment for kids, theoretically improving outcomes, Martin said.
"We found that when we looked at the vital signs and basic lab tests on day one, the day they get to the hospital, we could predict who was going to go on to develop more severe disease."
Combined with the demographic findings, providers can likely assess lab results on numerous measures, from white blood cell counts to creatinine levels, and pinpoint high-risk patients at admission.
"So when patients walk in the door of the emergency department and test positive for COVID, if a clinician sees that they have one or more of these at-risk demographic categories, that should raise a little red flag," Martin said. "That might help them get to the ICU or get an antiviral therapy earlier rather than later."
Goal: deeper studies, tool development
With the study's data in hand, the race is now on for researchers to develop computational tools that could speed the course of COVID care in youth by automatically alerting clinicians to high-risk traits and lab results.
The National Center for Advancing Translational Sciences (NCATS) - an institute of the National Institutes of Health and supporter of the study - recently issued the challenge.
"The hope is, by creating a little bit of friendly competition, we can come up with the best tools possible to help identify which kids are in most need of help," Martin said.
Multiple research teams involved in the study by the National COVID Cohort Collaborative (N3C) are already working on tools, including his own group of scientists at the CU Anschutz Medical Campus, Martin said.
"While the study confirms that, overall, kids do very well, there are groups of children who are at risk of getting really sick and even dying." - Blake Martin, MD
Tell Bennett, MD, MS, the head of Martin's team, has launched a pediatric COVID-19 dashboard using N3C data. Bennett is the study's senior author and section head of Informatics and Data Science in the CU Department of Pediatrics.
The open resource and ongoing effort can help inform any youth-focused COVID-19-related research for scientists and allow the public to track pediatric COVID statistics throughout the pandemic, Martin said.
Researchers hope the findings spur subsequent studies that dig deeper into the reasons behind the demographic disparities of COVID-19 and its related MIS-C (multisystem inflammatory syndrome in children).
Comparing COVID-19 and MIS-C
For the study, researchers compared severe COVID-19 and MIS-C hospitalized cases, confirming that the serious organ-targeting MIS-C generally affects younger children (under 12). While rare, the syndrome that results from previous SARS-CoV-2 infection, was, in many ways, also more severe.
Nationally, nearly 7,000 cases of the SARS-CoV-2 complication have been reported to the Centers for Disease Control and Prevention, with reports showing over half of children require ICU admission and more than one-third experience shock. Oftentimes, children present with severe MIS-C without having known they had contracted the virus.
In the N3C study, 707 children had MIS-C. In addition to younger age, Black and obese children were disproportionately affected. PCCCs, however, were not identified risk factors in the severely sick group.
"It was actually patients who were young and healthy, who didn't have these complex chronic medical conditions," Martin said. "Which I think goes against what a lot of us think when we think of children and COVID-19: 'Oh, my kids are young and healthy; it won't affect them.'"
Just over 16% of MIS-C kids needed a ventilator compared to 6% of kids with COVID-19. Over a quarter, or 27% of the MIS-C patients, needed blood-pressure medications to help their hearts beat more effectively or keep their blood pressure up compared to 5% of kids with COVID. "So these kids are really sick," Martin said.
In addition to improved care for youth, Martin hopes the study inspires awareness and a drive to protect the community, especially its most vulnerable members.
"I think this should be a motivator for all of us to get vaccinated, to get our kids vaccinated, to keep our kids home when they are having symptoms, because if we pass along this virus, there's a risk that somebody we know in one of these categories ends up getting really sick. Thankfully, the mortality rate is low. But it's not zero."






