Beneficial gut microbes and the body work together to fine-tune fat metabolism and cholesterol levels, according to a new preclinical study by investigators from Weill Cornell Medicine and the Boyce Thompson Institute at Cornell's Ithaca campus.
The human body has co-evolved with the beneficial microbes that live in the gut (termed the microbiota), resulting in mutually favorable relationships that aid in the digestion of food and absorption of essential nutrients required for survival of the host and the gut microbes. A central aspect of these relationships is the production of bioactive molecules that promote the breakdown of food, enabling nutrient absorption by the host. One of the most important groups of such molecules are termed bile acids (also known as "bile"), which are produced from cholesterol in the liver and then delivered to the intestine where they promote fat digestion.
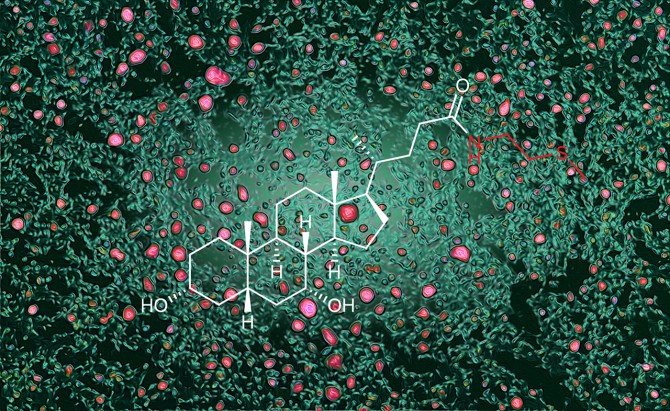
Lipid accumulation in a murine model of fatty liver disease, visualized by color-enhanced lipid droplets (pink) in liver tissue (green). Superimposed chemical structure of a newly discovered bile acid conjugate.
Scientists have known for some time that gut bacteria modify bile acids into a form that stimulates a receptor called FXR, which reduces bile production. The new study, published Jan. 8 in Nature, reveals that an enzyme produced by intestinal cells converts bile acids into a different form that has the opposite effect. This altered form, called bile acid-methylcysteamine (BA-MCY), inhibits FXR to promote bile production and help boost fat metabolism.
"Our study reveals there is a dialogue occurring between the gut microbes and the body that is vital for regulating bile acid production," said co-corresponding author David Artis, director of the Jill Roberts Institute for Research in Inflammatory Bowel Disease and the Friedman Center for Nutrition and Inflammation and the Michael Kors Professor in Immunology at Weill Cornell Medicine.
Bile acids help the digestive system break down fats into forms the body can take up and use. "But it now has become clear that bile acids are more than just digestive aids; they act as signaling molecules, regulating cholesterol levels, fat metabolism, and more," said co-corresponding author Frank Schroeder, a professor at the Boyce Thompson Institute and a professor of chemistry and chemical biology in the College of Arts and Sciences. "They do all this by binding to FXR, which acts like a traffic light, controlling cholesterol metabolism and bile acid production to avoid excess buildup."
Now the cross-campus collaboration between the laboratories of Schroeder and Artis has revealed the body's role in this fundamental biological process.
The study was co-led by Dr. Tae Hyung Won, a former postdoctoral associate in Schroeder's lab and now assistant professor at Cha University in South Korea; Dr. Christopher Parkhurst '02, an instructor of medicine at Weill Cornell Medicine, working in Artis' lab; and Mohammad Arifuzzaman, an assistant professor of immunology in medicine at Weill Cornell Medicine.
Artis and Schroeder used a technique called untargeted metabolomics to identify all the molecules produced by mice with and without gut microbes. By comparing the two, they were able to distinguish which molecules were made by the gut microbes and which were produced by the body. BA-MCYs stood out as molecules that were produced by the mice but were nevertheless dependent on the presence of gut microbes.
"The BA-MCYs demonstrate a new paradigm: molecules that are not produced by the gut microbes but are still dependent on their presence," co-first author Dr. Won said. Through a series of experiments, the investigators then showed how the body makes the BA-MCYs and how these molecules provide a way for the body to counteract the microbe's signals to produce less bile acid, preventing the slowdown of cholesterol metabolism.
"This balancing act is crucial," Schroeder said. "When gut bacteria produce lots of bile acids that strongly activate FXR, the body pushes back by making BA-MCYs, ensuring the bile acid system stays balanced."
The researchers also showed in their preclinical model that boosting BA-MCY levels helped reduce fat accumulation in the liver and that increasing intake of dietary fiber also enhanced BA-MCY production. "Importantly, BA-MCYs were also detected in human blood samples, indicating that a similar mechanism may occur in people," Arifuzzaman said.
The investigators said their study approach may also help researchers study the role of the gut microbiota in a wide range of diseases, from infection and chronic inflammation to obesity and cancer.
"Our paper is a roadmap to using untargeted metabolomics and chemistry to better understand how the dialogue between the gut microbiota and the body impacts a range of diseases," Artis said.
Support for this research came from grants from the National Institutes of Health; the Allen Discovery Center program; the Kenneth Rainin Foundation; Cure for IBD; Howard Hughes Medical Institute; the Sanders Family; the Rosanne H. Silbermann Foundation; Glenn Greenberg and Linda Vester Foundation; and Weill Cornell Medicine Jill Roberts Institute.
Bridget Kuehn is a freelance writer for Weill Cornell Medicine.