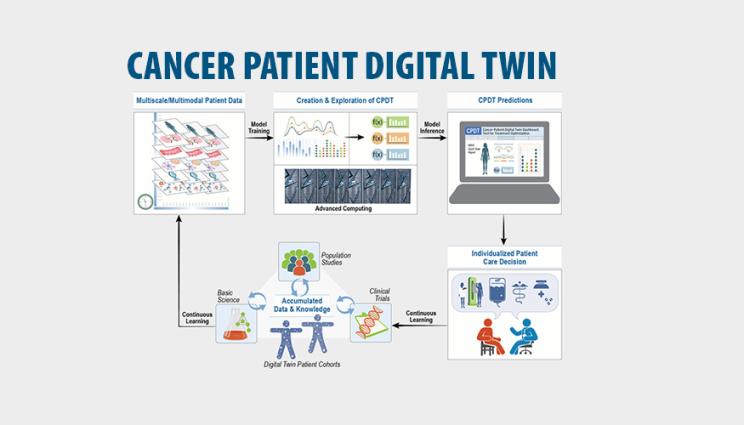
A proposed framework for Cancer Patient Digital Twins (CPDTs) - virtual representations of cancer patients using real-time data - would combine high performance computing modeling and simulation, model inference and clinical data to make treatment predictions and individualized health care decisions for cancer patients. Illustration by Jeannette Yusko and Janelle Cataldo/LLNL.
A multi-institutional team, including a Lawrence Livermore National Laboratory (LLNL) contributor, has proposed a framework for digital twin models of cancer patients that researchers say would create a "paradigm shift" for predictive oncology.
Published online in Nature Medicine on Nov. 25, the proposed framework for Cancer Patient Digital Twins (CPDTs) - virtual representations of cancer patients using real-time data - would combine high performance computing modeling and simulation, model inference and clinical data to make treatment predictions and individualized health care decisions for cancer patients. When fully realized, CDPTs would reflect a patient's molecular, physiological and lifestyle characteristics as they evolve over time and across different treatments, and help "usher in a new age in medicine" by increasing the probability of optimal care, the authors concluded.
"CPDTs are a grand challenge problem in this growing convergence of high performance computing and oncology," said contributor Amy Gryshuk, who serves as a lead in LLNL's Strategic Science Engagements Office. "They have a tremendous potential to advance predictive medicine, but to fulfill that promise we will need to integrate multiscale and multimodal data to then build and test dynamic models at scale."
The CDPT concept stems from a partnership between Department of Energy laboratories, the National Cancer Institute (NCI), academia and industry, who formed the Envisioning Computational Innovations for Cancer Challenges (ECCIC) community in 2019. LLNL hosted the first ECCIC meeting - co-organized by Gryshuk - which investigated the crossroads of advanced computing and cancer research and birthed the idea.
Under the proposed framework, researchers would create a multiscale and multimodal dataset from individual-level patient data, as well as clinical trials and population studies, to train mechanistic and artificial intelligence (AI) models. It would address changes across timescales from the molecular level to the population level, and as the patient's disease state evolves, the digital twin would incorporate real-time observational data to predict future states.
Researchers envision clinicians will use CPDTs to perform virtual experiments, simulating the patient's disease trajectory under different treatments. At each visit with a clinician, the predictions would be compared with real-life measurements to assess the digital twin's performance and update it in a "continuous learning" loop to inform patient decision making.
In addition to individual patient predictions, CPDTs will provide policymakers with insights into which cancer therapies show the most promise, informing investment and resource allocation and helping healthcare systems better respond to public health situations in real time, researchers reported.
While CPDTs could revolutionize how cancer and a host of other complex diseases are treated and managed, authors cautioned that the scientific community would need to overcome hurdles in data, modeling and integration, as well as ethical concerns. Data will need to be captured across diverse populations and under FAIR (Findability, Accessibility, Interoperability, Reusability) principles to ensure they do not reinforce pre-existing biases, the team concluded.
The paper involves researchers at Stanford University, Indiana University and the NCI, and includes co-authors at the Frederick National Laboratory for Cancer Research, the IBM Almaden Research Center and the Institute for Systems Biology.






