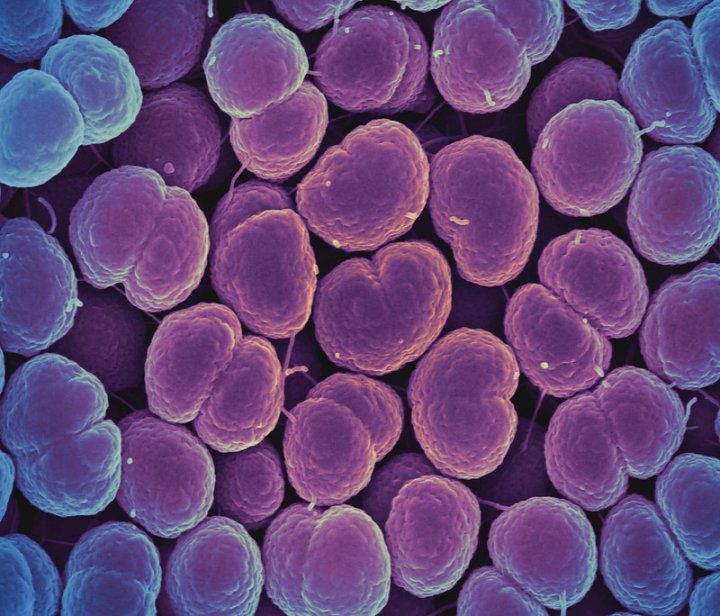
A significant proportion of bacterial sexually transmitted infections (STIs) - gonorrhea, chlamydia, or syphilis - were prevented with a dose of doxycycline after unprotected sex, according to preliminary results of a clinical trial that closed early because it was very effective for men who have sex with men and transgender women who are living with HIV or are taking HIV pre-exposure prophylaxis (PrEP).
The results of the clinical trial, conducted in San Francisco and Seattle, have been eagerly anticipated by public health officials and clinicians who are looking for new ways to prevent STIs, which have been on the rise in the United States and many other parts of the world for the past six years.
Researchers examined an approach known as doxycycline post-exposure prophylaxis (or DoxyPEP), in which people take 200 milligrams of the antibiotic doxycycline within three days of having sex without a condom.
They recruited from public health clinics in San Francisco and Seattle. To qualify, participants had to have had gonorrhea, chlamydia or syphilis, in the previous year. Participants were randomized to receive doxycycline or no doxycycline in an open-label study design.
The trial was designed to allow an independent team monitoring the trial's safety to look at interim results, to see if the intervention proved effective enough that it could be stopped early. Data from 554 participants showed that those who were randomized to take doxycycline had substantially fewer infections than those who did not receive doxycycline, and this reduction in STIs occurred both in participants taking HIV PrEP as well as those living with HIV. Doxycycline was generally safe and well tolerated.
Researchers said the data support the effectiveness of DoxyPEP to prevent STIs in the population they studied.
"At this point, doxycycline after sex is a targeted intervention for certain populations, in this case men who have sex with men or transgender women who have already had an STI in the past year," said Annie Luetkemeyer, MD, a professor of infectious diseases at UC San Francisco. She led the study with Connie Celum, MD, professor of global health, medicine, and epidemiology at the University of Washington School of Medicine.
"Doxycycline as PEP may be similar to HIV PrEP, which isn't for everyone, but is an effective strategy for those at increased risk for HIV infection," Luetkemeyer said. "Future recommendations for doxycycline use as an STI prevention strategy will need to consider effectiveness in different populations, as well as antimicrobial resistance."
The trial has yet to determine whether intermittent use of doxycycline may lead to increased antibiotic resistance in the bacteria that cause STIs or that naturally live on the body, and whether it may lead to negative changes in the bacteria of the gut.
Researchers will present updated effectiveness and adherence data from the approximately 630 participants who were enrolled by the time the study closed, along with antibiotic resistance data at AIDS 2022, the 24th International AIDS Conference in Montreal, Canada and virtually July 29 to August 2.
The trial was funded by the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health, through grant R01AI143439, and conducted at the HIV clinic at Zuckerberg San Francisco General Hospital and the San Francisco City Clinic, both part of the San Francisco Department of Public Health, and the Madison Clinic and the Sexual Health Clinic at Harborview Medical Center, both at the UW Medicine.






