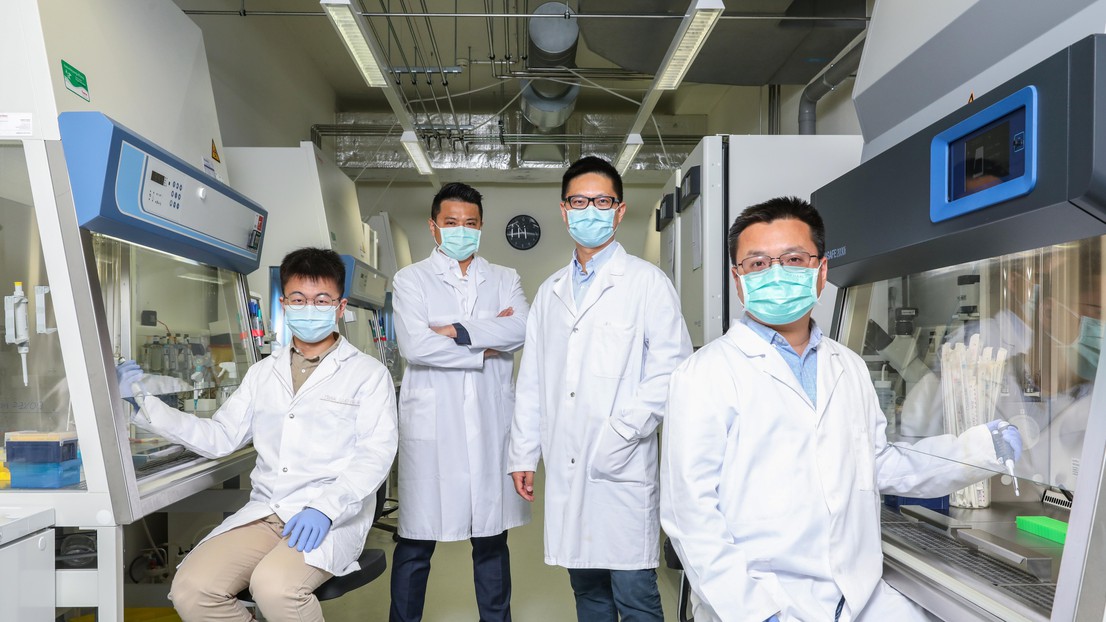
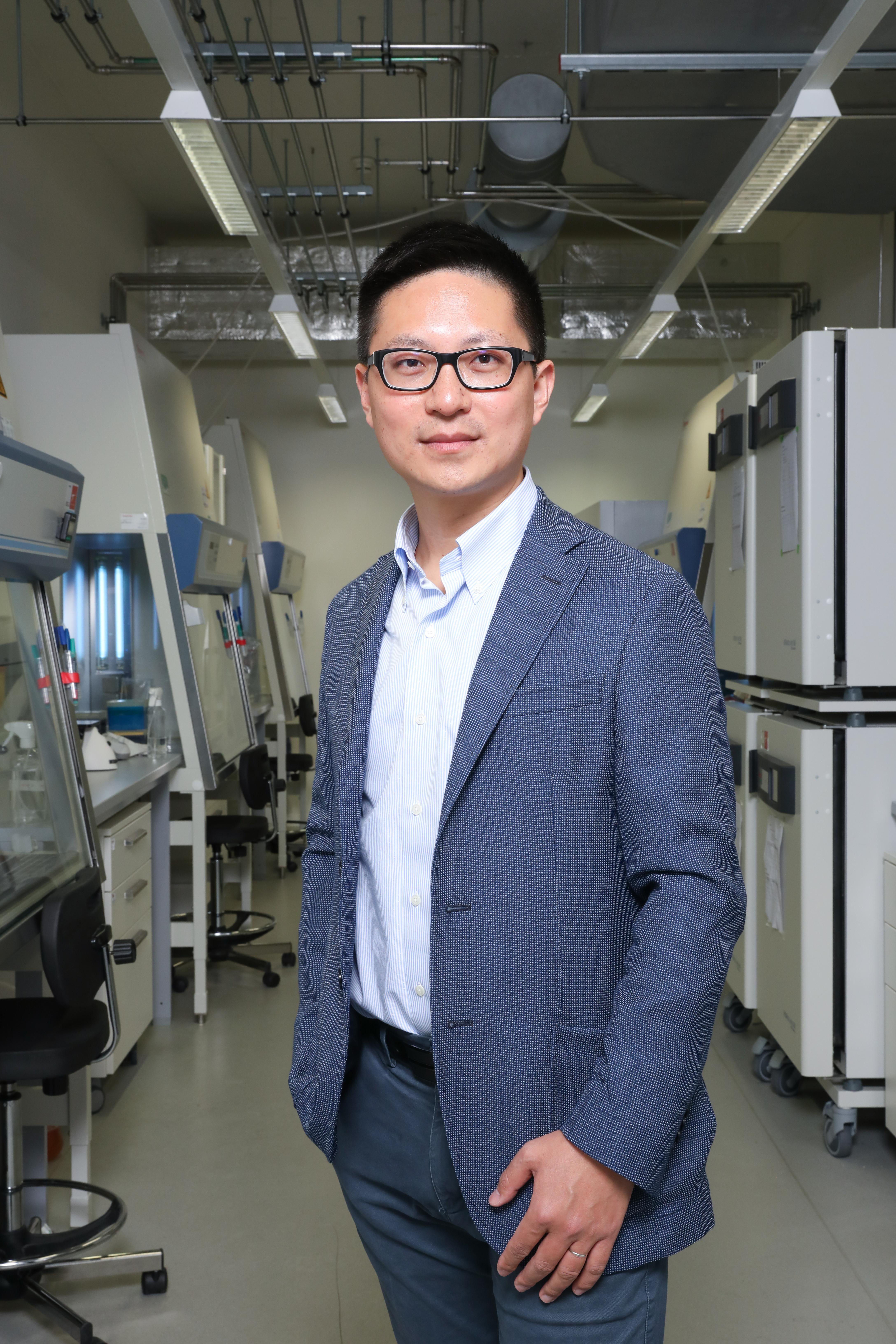
Ping-Chic Ho, Yu-Qing Xie, Yugang Guo and Li Tang © Alain Herzog / 2021 EPFL
EPFL scientists have discovered that an engineered interleukin-10-Fc fusion protein can boost the effectiveness of exhausted T lymphocytes - our body's immune cells for fighting cancer, by reprograming their metabolism.
One of the many treatment options available for cancer today is immunotherapy, which involves stimulating a patient's immune system to produce lymphocytes (such as T cells) that go on to kill the tumor. Without immunotherapy, a patient's lymphocytes are generally powerless against the disease. This form of treatment has shown to be effective, but it has a major drawback: it works on only 20-30% of patients. A majority of cancer pateints do not benefit from current cancer immunotherapies.
Teamwork
Researchers around the world are working hard to increase that percentage. At the Laboratory of Biomaterials for Immunoengineering led by Prof. Li Tang, within EPFL's Institute of Bioengineering and School of Engineering, a group of scientists has led the joint efforts of six research labs at universities in different countries to study a new method for making immunotherapy more effective. The international team - comprised of 22 experts in fields ranging from biology and immunology to bioengineering and biocomputing - has just published their findings in Nature Immunology.
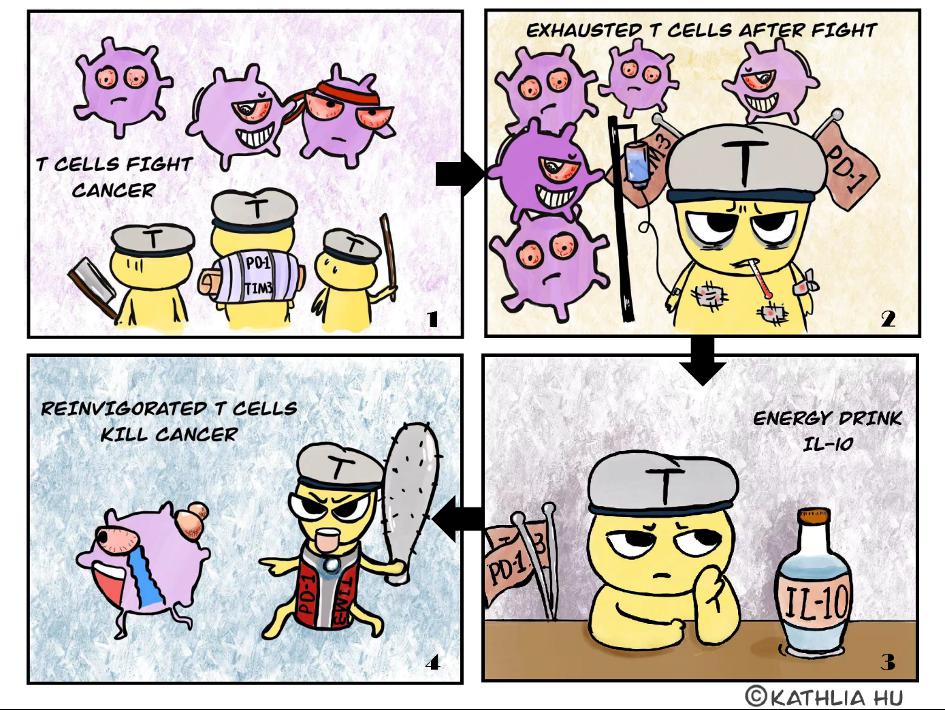
Boosting tired T cells
"The majority of cancer patients don't respond to immunotherapy - that's a major obstacle we need to overcome," says Tang. "One explanation could be that the process of infiltrating a tumor and fighting cancer cells wears out the lymphocytes, making them too tired to halt the tumor's progression. The scientific term for that is 'T cell exhaustion'. The cells are not - or are no longer - responsive to immunotherapy."
The scientists' new method involves adding a newly engineered protein called interleukin-10-Fc fusion proteinto immunotherapy drugs. "Interleukin-10 can boost or suppress our immune system depending on the scenario. However, very little was known how exactly it interacts with tumor-infiltrating T cells until our research," says Yuqing Xie a doctoral assistant at Tang's lab. "But we seem to have found a new mechanism which could revitalize exhausted T cells." Their tests indicate that interleukin-10-Fc acts as an energy booster, giving lymphocytes a second impetus so they can be reactivated and keep fighting tumors. Dr. Yugang Guo, a scientist at Tang's lab, explains: "With this protein we are able to reprogram T cell metabolism and enhance their expansion and destructive capacity against cancer."
Up to 90% healing rate
The method was tested on mice with unequivocal results - up to 90% of the diseased animals were able to defeat the cancer. "Interleukin-10-Fc appears to be highly effective. It works in synergy with adoptive T cell transfer immunotherapy, such as CAR-T therapy, or immune checkpoint inhibitors, leading to the eradication of established solid tumors and durable cures in a majority of treated mice. Our method seems to improve the existing immunotherapies against solid tumors, which are known to be difficult to be cured" says Tang. What's more, no obvious side effects were observed during the tests, which bodes well for clinical trials in the future. The researchers Dr. Yugang Guo, Yuqing Xie and Prof. Li Tang have filed international patents of this new therapy and will soon be pushing it to clinical trials on patients.
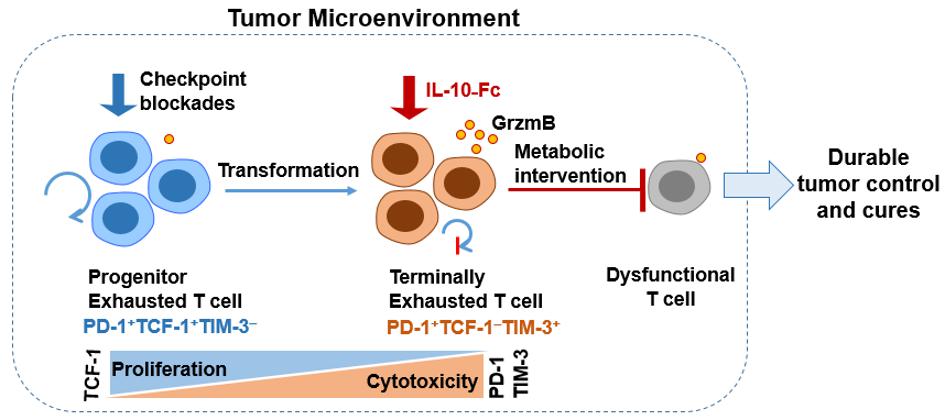
Bottleneck breakthrough
Among the tumor infiltrating T cells, a subset called 'terminally exhausted CD8+ T cell', does not respond to most existing immunotherapies including immune checkpoint blockades. It is known to be difficult to be reactivated. The study, led by Prof. Li Tang, shows that metabolic reprogramming of these cells through a molecule, called mitochondrial pyruvate carrier, is sufficient to restore the functionality of terminally exhausted CD8+ T cells for fighting cancer. This finding lays the foundation for further identification of metabolic stimulations that are needed for reinvigorating terminally exhausted CD8+ T cells, a current major bottleneck in the field of cancer immunotherapy.






