Examining the immune cells in the environment around a tumour could help to predict how a person's cancer might progress and respond to treatment, according to new research led by UCL and the Francis Crick Institute.
The study, published in Cancer Discovery and reported at the American Association for Cancer Research Annual Meeting 2024, is part of the Rubicon project, which aims to create a detailed map of lung cancer immunology to speed up the development of new treatments.
The team classified four different environment subtypes found around lung tumours, each associated with different patterns of cancer progression. Cancers identified as having low levels of immune infiltration by T and B cells, but high levels of neutrophils, were more likely to spread to other parts of the body.
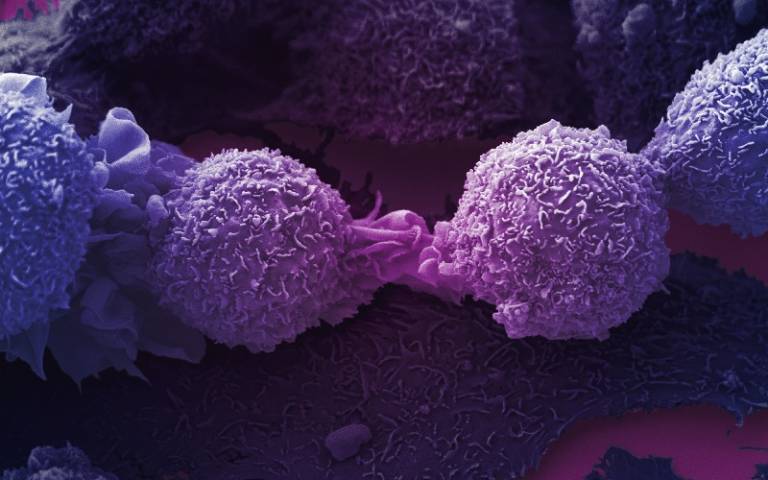
The tumour microenvironment is a mixture of cancer cells, immune cells, structural proteins and blood vessels. Because the makeup of the microenvironment can vary throughout and around the tumour, looking at multiple sites of the tumour and its surroundings is helpful to get a more accurate picture of what is happening during disease progression.
The researchers used advanced imaging techniques to map single cells and outline four different microenvironments in lung cancer, by investigating samples of tumours and normal tissue from 81 patients with non-small cell lung cancer (NSCLC) taking part in the TRACERx study.
They looked at T and B cells, macrophages and neutrophils, which are all types of white blood cell involved in immune response. Each class of microenvironment is composed of varying numbers of immune cells in different areas of the tumour:
- 28% of tumours had a very active immune environment, with high numbers of T and B cells and macrophages in the inner and outer parts of the tumour. These were described as 'immune hot'.
- 24% of tumours had a low infiltration of T cells and macrophages in the inner part of the tumour, but many B and T cells in the outer part of the tumour, without many macrophages.
- 17% of tumours had a less active immune environment, with low numbers of T and B cells and macrophages throughout the tumour.
- 19% of tumours had a low infiltration of T and B cells and macrophages throughout the tumour, but a large number of neutrophils.
In the fourth subtype, identified as having high levels of neutrophils, the researchers observed that tumours were also further away from a reliable blood supply. Subsequent evolutionary changes in these tumours enabled evasion from the T and B immune cells that are able to attack the cancer.
By comparing tumours likely and unlikely to spread, the researchers saw that the number of neutrophils was higher in tumours that were more likely to spread. They then used statistical and machine learning methods to confirm this association.
The results suggest that measuring the number of neutrophils could be an effective clinical test, helping clinicians to determine who might need additional treatment to prevent cancer spread.
Mihaela Angelova, a postdoctoral fellow in the Cancer Evolution Laboratory at the Crick and co-senior author of the study, said: "We've shown that high infiltration of neutrophils could be a marker for cancer evolution and spread. These tumours were genetically altered, separated from the blood supply and managed to evade the immune system, making them better able to spread."
Professor Charlie Swanton, co-senior author of the study from UCL Cancer Institute, Head of the Cancer Evolution Laboratory at the Crick and Chief Clinician at Cancer Research UK, said: "Lung cancer, particularly if caught at a later stage, is hard to treat, and mapping the environment around the tumour can help us to categorise cancers and work out personalised treatment strategies for patients.
"This research highlights the importance of pairing the evolutionary history of a tumour with information on how the tumour microenvironment organises in 3D to build the most accurate picture of an individual's cancer."
The researchers are now investigating what happens to the tumour microenvironment as the cancer metastasises - spreads and becomes genetically varied throughout the body.
This project was led by co-first authors Katey Enfield, Emma Colliver, Claudia Lee and Alastair Magness, and involved collaborations with Erik Sahai and Julian Downward's laboratories, as well as Flow Cytometry and Experimental Histopathology technical teams.
The Rubicon study is an Investigator-Sponsored Research (ISR) study, funded by Bristol Myers Squibb, and the TRACERx project is funded by Cancer Research UK.






