How many mutations do I, or any member of my species, need to improve our chances of survival? There is no single correct answer to that question, but one might think about it in terms of the inherent tension between innovation and conservation. If the mutation rate is high - that is, if more errors occur during replication of the genome from parent to offspring - the outcome will sometimes be advantageous for us, allowing us to adapt faster to our environment, but it may come at a heavy price. If we opt for a more conservative approach, however, with a slower mutation rate, we ensure that the status quo will be maintained, but we won't benefit from any new traits that could help improve the survivability of the chain.
Many researchers have asked these questions, but, until now, not in connection with new medical treatments that increase the mutation rate of viruses or bacteria with the goal of eradicating them. Rather surprisingly, the person who did raise the question in this context was not a scientist, but a social media user with a lot of common sense. He was responding to an encouraging announcement at the height of the coronavirus pandemic from the pharmaceutical company Merck. The company had received emergency, fast-track approval from the US Food and Drug Administration for a new drug called molnupiravir, which tricks the SARS-CoV-2 virus into mutating so quickly that it kills itself off. The man's logical response: Although in most cases it is clear that speeding up the mutation rate will be fatal for viruses, every so often viruses could benefit from the changes to their genome, which could give them improved capabilities - and then humans would encounter more dangerous strains of coronavirus and end up paying a heavy price for this evolutionary innovation.
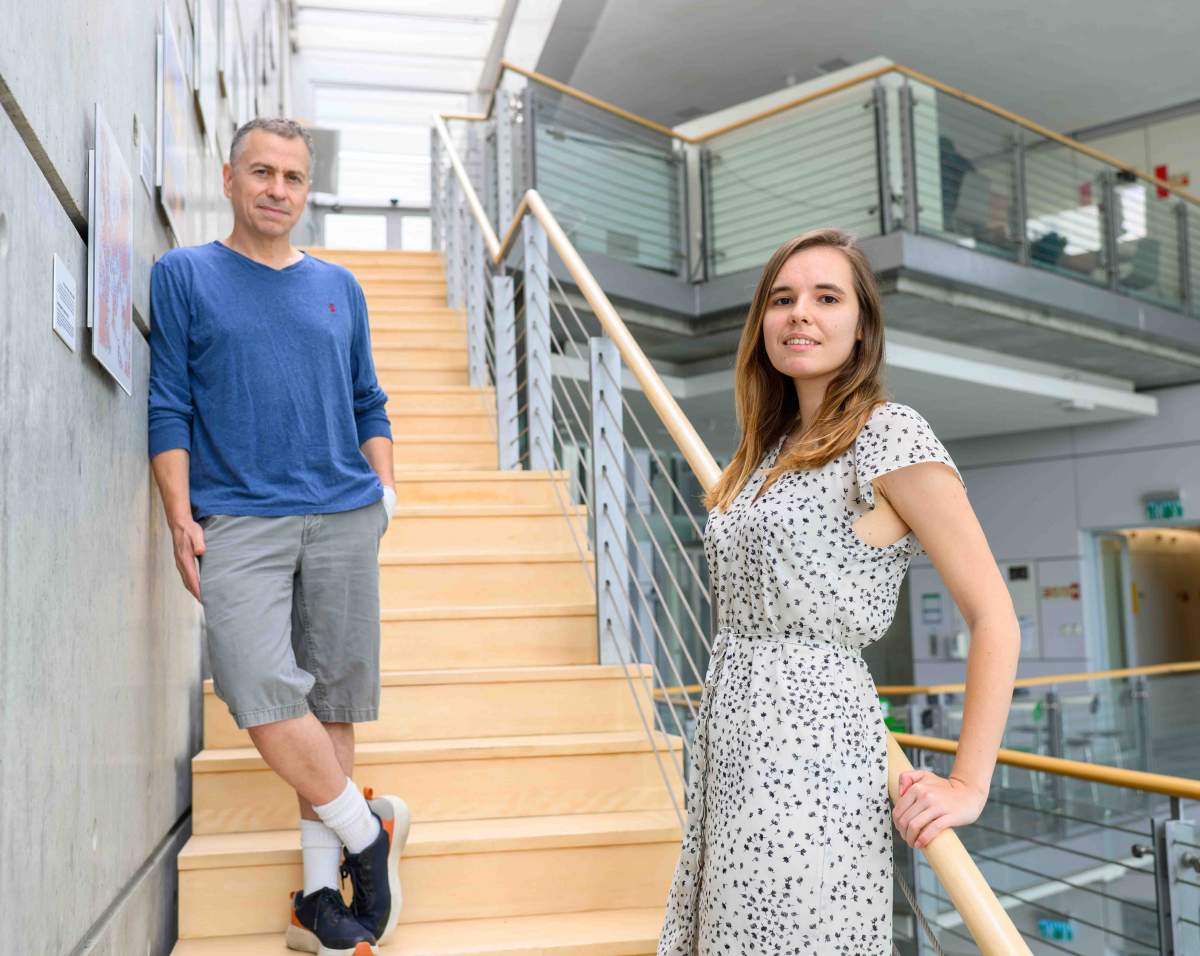
Prof. Yitzhak Pilpel from the Weizmann Institute of Science's Molecular Genetics Department saw that social media post and wondered: Is it possible that the drug has a very serious flaw that was overlooked during the development and approval process? "As far as I know," Pilpel explains, "this is the first drug ever that was developed to kill the virus by accelerating the mutation rate as its key mechanism, and this could change the way that a lethal epidemic spreads. Since drug safety tests usually focus on their effect on the patients themselves - in other words, on the physiological safety of the drug - it seems that a need has arisen for a system that will test the safety of drugs from an entirely new perspective, which will impact the entire human population: evolutionary safety. Such a test would also be relevant for drugs - developed before molnupiravir - that also accelerate the mutation rate of viruses or bacteria, but do so as an unintended byproduct."

Working with doctoral student Gabriela Lobinska from his own laboratory and Prof. Martin A. Nowak from Harvard University, Pilpel began looking for ways to deal with the challenge of developing a new kind of test. The researchers suggest three possible ways of testing for evolutionary safety. The first is to make the test part of the clinical trials for new drugs. While this is a thorough way of identifying interactions between the pathogen and the patient, it may be too complex to perform, in part because of the need to track the multiple branches of the lineage of viruses or bacteria. At the same time, because of the limited size of the test group receiving medical treatment, it would only reflect a small number of the mutations and could even miss those that led to the extinction of the pathogen and therefore did not survive in the patient. The second system of testing for evolutionary safety could be conducted in the laboratory and is expected to provide a much fuller picture of the subsets of mutations, including those created following different types of treatment, such as varying doses of the drug.
""We urge regulatory bodies and pharmaceutical companies to incorporate evolutionary safety concerns into the development and authorization process for new drugs"
The researchers, however, focused on the third research paradigm: a theoretical test using a mathematical model capable of presenting a comprehensive picture of the lineage of the viruses or bacteria and how they responded to medical treatment. The scientists formulated a computational template that allowed them to analyze tens of thousands of possible mutations in the coronavirus's genome. The goal was to assess the respective likelihood of three possible situations: a mutation that is beneficial for the virus and detrimental to humans, such as one that improves infectiousness or increases resistance to existing drugs; a mutation that is lethal for the virus and beneficial for us; and cases where the mutation does not lead to any significant changes in the virus's genome.
In a scientific paper recently published in PLOS Biology, the researchers concluded that Merck's drug could be a double success. It healed people with coronavirus, and the current model suggests it might also be good for humanity under certain conditions, as it might lower the risk that new worrisome strains would emerge. The secret is in the numbers. The study found that, when it comes to evolutionary safety, the number of mutations that were good for the virus but bad for humans was of limited significance. If a drug increases the number of changes in the genome of the virus but decreases its population at a rapid rate, the evolutionary risk posed by this drug will be low. At the same time, it is important to take into account the fact that the strength of the patient's immune system and the timing of the start of treatment also have a major impact on evolutionary safety.
Science Numbers
Molnupiravir increases the rate of copying errors during the replication of the coronavirus from 1 per 1,000,000 without treatment to 2 or 3 per 1,000,000 after treatment. The drug reduces the viral load by a factor of 10, and the hospitalization rate, by 33%. According to the new study, treatment might also reduce the emergence risk of a particularly virulent viral strain by about 50%.
"We urge regulatory bodies and pharmaceutical companies to incorporate evolutionary safety concerns into the development and authorization process for new drugs," the researchers say. "A better understanding of the use of accelerated mutation rates in therapy will turn this approach into a valuable ally in the battle to eradicate diseases. It will help us more accurately predict the emergence of new strains and design drugs that will not only ensure patient recovery but will also be safe for the entire population."
Prof. Yitzhak Pilpel's research is supported by the Helen and Martin Kimmel Award for Innovative Investigation. He is head of the Braginsky Center for the Interface between Science and the Humanities; head of the Azrieli Institute for Systems Biology; head of the Leo and Julia Forchheimer Center for Molecular Genetics; and head of the Kahn Family Research Center for Systems Biology of the Human Cell. Prof. Pilpel is the incumbent of the Ben May Professorial Chair.






