Illawarra researchers awarded close to $1.5 million from FightMND
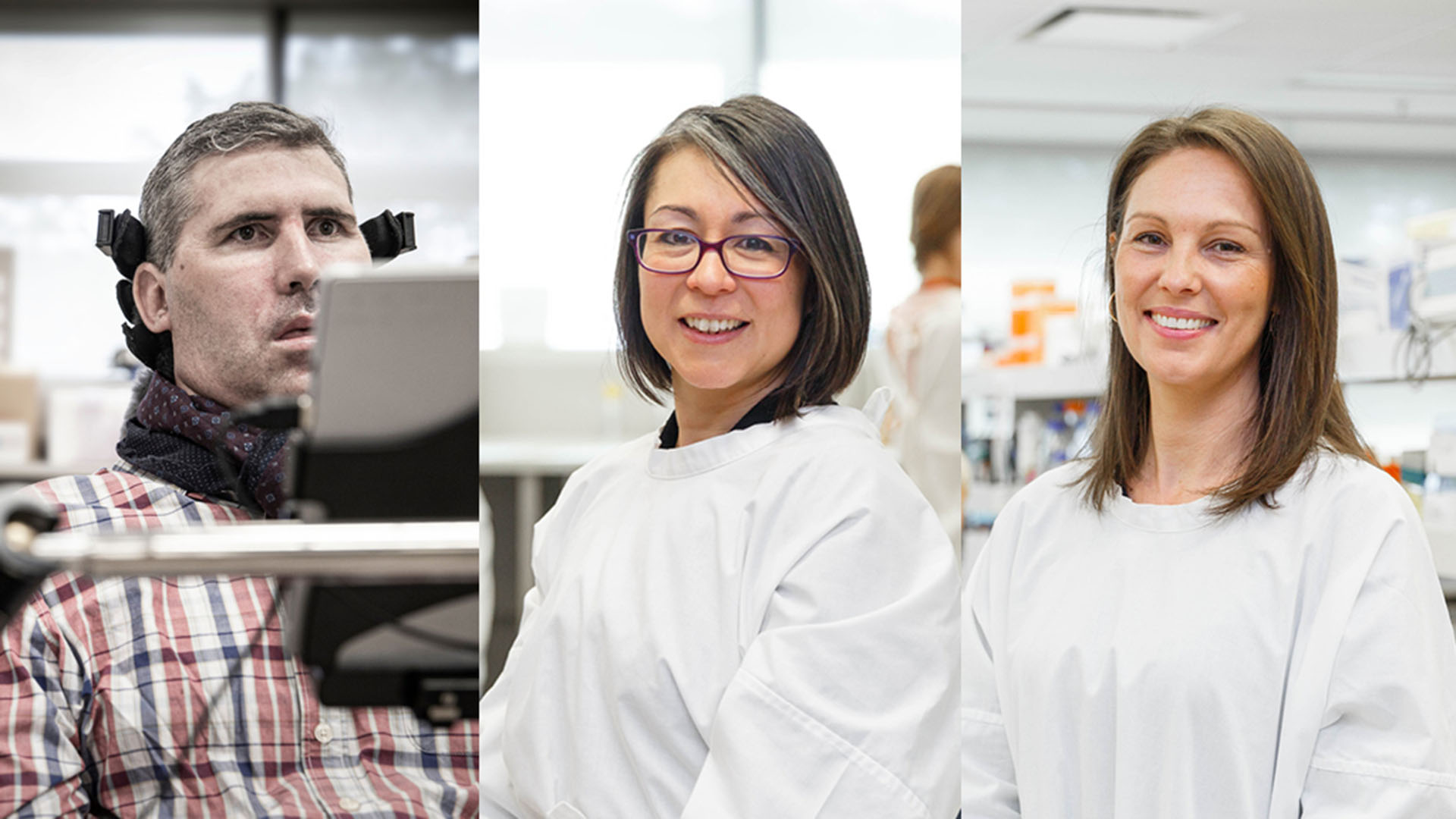
Three researchers from the Illawarra Health and Medical Research Institute (IHMRI) and the University of Wollongong (UOW) have received a share of $1.5 million from FightMND to investigate potential treatments for motor neurone disease (MND).
MND is a terminal neurodegenerative disease with no current cure or effective treatment options. The rapidly progressive disease causes motor neurones, the pathways between the brain and muscles, to degenerate and die. As a result, MND leaves patients with the inability to walk, talk and eventually breathe.
Professor Justin Yerbury has been awarded a Drug Development Grant for nearly $1million for the second year running. His latest research project will test a gene therapy in collaboration with ProMIS Neurosciences that targets misfolded proteins associated with familial MND.
Misfolded SOD1 proteins are associated with some forms of MND, and current leading therapeutic strategies are looking to knock down the SOD1 protein levels. However, in the long term this can contribute to other medical complications.
"We have designed an artificial gene encoding an enzyme that selectively targets the mutant form of SOD1 for disposal but spares the normal SOD1 protein," said Professor Yerbury.
We hope that if successful, this potential therapeutic strategy could increase the average length of patient survival after diagnosis, which for many is currently only between one to five years.
Dr Kara Vine-Perrow is a co-investigator on this project with Professor Yerbury, in addition to being awarded an Impact Grant for $250,000 to develop targeted drug delivery technology to treat MND.
"We have designed a drug carrier that can increase the delivery of drugs into the brain. We now wish to enhance the penetration and targeting capabilities of this using non-invasive focused ultrasound," said Dr Vine-Perrow.
Focused ultrasound is a safe and relatively new technique that selectively disrupts the body's blood-brain barrier and blood-spinal cord barrier, increasing its permeability to drugs into targeted regions within the central nervous system.
"This barrier is a major obstacle facing the effective treatment of diseases such as MND, making it near impossible for therapeutic drugs to target the diseased cells. If we can overcome this barrier and improve drug delivery to the brain and spinal cord where it is needed, it could lead to improved outcomes for people living with MND," said Dr Vine-Perrow.
Associate Professor Lezanne Ooi was also awarded an Impact Grant for $250,000 to test a combination therapy designed to prevent the toxic effects of the TDP43 protein, which is responsible for a host of functions in the cell. If successful, it has the potential to restore motor neurone function and survival.
"If TDP43 can be modulated to slow toxic protein aggregates from forming and to restore healthy neuronal function, this could provide enormous therapeutic benefit to patients," Professor Ooi said.
The prevalence of MND internationally is estimated to be between 3 - 7 people per 100,000 but the rapid progression of the disease means that the lifetime risk is around 1:400.
All grant funding was provided by FightMND, a not-for-profit established with the purpose of finding effective treatments and ultimately a cure for MND. Their flagship fundraising event, The Big Freeze, raises close to $15 million and plays a significant role in raising community awareness of MND.
"FightMND has been a game changer for the development of therapies for MND and the study of MND more generally in Australia," said Professor Yerbury.






