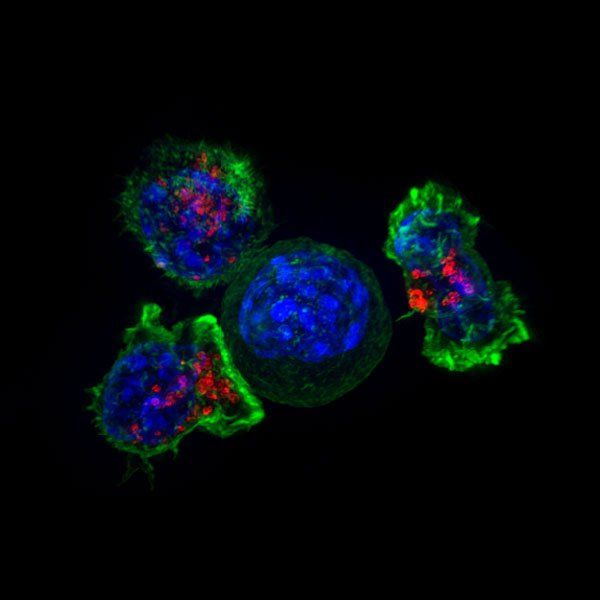
T cells used in immunotherapy treatments can get exhausted by the task of fighting cancer cells or get shutdown as they enter tumors. Using a CRISPR-based edit on these cells' genomes, researchers at UC San Francisco and Gladstone Institutes have rendered the therapeutic cells more resilient. The discovery may help overcome a major factor limiting the success of these promising therapies in curbing both solid and liquid tumors.
"We've succeeded in engineering better, stronger, longer-lived T cells that we think will improve treatment of both blood and solid cancers," said Alex Marson, MD, PhD, who, along with cancer biologist Alan Ashworth, PhD, FRS led the study, published in Nature on Aug. 24, 2022. "It's an example of how we're using the power of CRISPR to accelerate the design of improved T-cell therapies."
Marson also heads up the Gladstone-UCSF Institute of Genomic Immunology, a joint effort of the two institutions to bring a combination of advanced genomic technologies to bear on the creation of new cell-based immunotherapies.
"These genomic innovations are creating avenues to tackle the challenges of developing highly effective and precisely targeted immunotherapies," said Ashworth, president of the UCSF Helen Diller Family Comprehensive Cancer Center. "The capacity to direct cell behavior by manipulating the genome will likely lead to transformational changes in the treatment of many diseases."
One of the major challenges of developing highly effective cancer immunotherapies is the fact that tumors exist in an environment that suppresses T cells and other immune cells, allowing the tumor to form and grow. Therapeutic T cells, engineered from a patient's own T cells to recognize and kill tumor cells, often get exhausted or dysfunction as they battle this environment, becoming unable to take down the cancer cells.
"By knocking out one individual gene, we've created cells that are not just potent tumor cell killers but also more persistent killers over a long period of time," said physician-scientist Julia Carnevale, MD, a corresponding author on the study, who has recently started her own lab in UCSF's Department of Medicine, pursuing new strategies to engineer superior cell therapies for cancer treatment.
An Unexpected Target
Using a set of CRISPR screens that allowed them to turn off each gene in the genome, one at a time, in a pool of human T cells, the team found a handful of candidates that could render the T cells resistant to key aspects of the immune-suppressive microenvironment often found in tumors.
Carnevale, who is also an affiliate investigator at Gladstone, and co-corresponding author Eric Shifrut, PhD, were particularly intrigued by one gene named RASA2, because it had never been associated with immune cell function before.
The capacity to direct cell behavior by manipulating the genome will likely lead to transformational changes in the treatment of many diseases.
"This was uncharted T-cell biology," said Shifrut, a former postdoctoral scholar in the Marson lab and now assistant professor at Tel Aviv University. "By focusing on RASA2, we wanted to find out whether controlling expression of the gene in human T cells might make them more sensitive immunotherapy agents."
Leveraging models created by corresponding authors Giedre Krenciute, PhD, of St. Jude Children's Research Hospital and Justin Eyquem, PhD, the team created T cells with the RASA2 gene knocked out. They then subjected these T cells to various "stress tests" by exposing them repeatedly to cancer cells as well as to models of the tumor microenvironment.
They compared the performance of these cells to that of the original therapeutic T cells that still contained a functioning RASA2 gene. Long after the original cells had lost their cancer-fighting abilities, the cells with RASA2 knocked out remained remarkably tireless.
The results were consistent in tests on different types of engineered T cells in which the team had blocked RASA2, and across cells from many different human donors and in models of both liquid and solid cancer.
"The knockout cells could just keep killing," said Carnevale. "It seems as if we found the brake in the system and when we take it off, we unleash the potential of these therapeutic cells."
Improving Existing Therapies
Now that Carnevale has a promising target, she and her colleagues are investigating it in preclinical models to streamline its effectiveness and assess its safety, a vital aspect of the research, said Shifrut.
"We want to ensure that when we remove RASA2's braking effect, the T cells only recognize and attack cancer cells, and not healthy cells," he said.
In collaboration with other labs at the institute, the researchers are laying the groundwork for a clinical trial by combining multiple novel technologies with RASA2 deletion, to improve an already-existing T-cell therapy.
"Even in the best-case scenarios, immunotherapy treatments don't work for all patients and there are many examples of relapse," Carnevale said. "If we can push the boundary of this therapeutic approach by figuring out the right ways to rewire T cells, that would be really exciting."
Carnevale and Shifrut credited the unbiased and methodical CRISPR screening method for uncovering this unsuspected gene, saying the approach points the way to unconsidered biology and broadens the impact of studies like these.
Marson agreed. "This study taught us that RASA2 has roles in immunology that had previously been unexplored," he said. "Similar systematic studies, using CRISPR to look at every gene in the genome, will not only accelerate design of cancer therapies, but should also aid in designing cellular medicines that are better at treating all kinds of conditions, from autoimmune disorders to infectious disease."
Authors: Additional authors on the study include William A. Nyberg, Franziska Blaeschke, Yan Yi Chen, Zhongmei Li, Shane Vedova, Stefanie Bachl of the Gladstone-UCSF Institute of Genomic Immunology, as well as Nupura Kale, Bindu Hegde, Scott Kogan, Hideho Okada, Kevin Shannon, Sagar P. Bapat, Morgan E. Diolaiti, and Patrick O'Leary of UCSF, Ansuman Satpathy, Julia Belk, Bence Daniel, and Theodore L. Roth of Stanford, Alejandro Allo Anido, Brooke Prinzing, Jorge Ibañez-Vega, Shannon Lange, Dalia Haydar, Marie Luetke-Eversloh, Maelys Born-Bony, and Stephen Gottschalk of St. Jude Children's Research Hospital, and Tobias Feuchtinger of Dr. von Hauner Children's Hospital, University Hospital, LMU Munich, Germany.
Funding: This work was supported by NIH grants 1K08CA252605-01 R01NS106379-02, R01CA173750, R01NS121249, K99CA256262, P30CA021765, 1S10OD010786-01, and P30CA082103, as well as the Cancer Research Institute, Parker Institute for Cancer Immunotherapy, and other institutes and philanthropy. For a complete list, please see the study.
About UCSF: The University of California, San Francisco (UCSF) is exclusively focused on the health sciences and is dedicated to promoting health worldwide through advanced biomedical research, graduate-level education in the life sciences and health professions, and excellence in patient care. UCSF Health, which serves as UCSF's primary academic medical center, includes top-ranked specialty hospitals






