PHOENIX - Mayo Clinic announces the results of an innovative treatment approach that may offer improvement in overall survival in older patients with newly diagnosed glioblastoma while maintaining quality of life. Glioblastoma is the most lethal type of primary brain cancer due to its aggressive nature and its treatment-resistant characteristics. It is the most common form of primary brain cancer. Each year an estimated 14,500 people in the U.S. are diagnosed with the disease. Results of Mayo Clinic's phase 2, single-arm study are published in The Lancet Oncology.
Sujay Vora, M.D., radiation oncologist at Mayo Clinic, led a team of researchers investigating the use of short-course hypofractionated proton beam therapy incorporating advanced imaging techniques in patients over the age of 65 with newly diagnosed World Health Organization (WHO) grade 4, malignant glioblastoma.
Results showed that 56% of participants were alive after 12 months and the median overall survival was 13.1 months." As compared to prior phase 3 studies in an older population having a median survival of only six to nine months, these results are promising," says Dr. Vora. "In some cases, patients with tumors that have favorable genetics lived even longer, with a median survival of 22 months. We are very excited about these results."
Glioblastoma is among the most challenging cancers to treat. The disease invades healthy brain tissue with hairlike tentacles, making surgical removal intricate. Surgeons must carefully balance removing as much of the tumor as possible while avoiding harm to critical areas of the brain responsible for essential functions such as movement and speech. Additionally, the tumor's cellular composition and its ability to evade therapies further challenge treatment efforts.
Standard radiation therapy is commonly used to treat glioblastoma and can be effective. However, a limitation is that it also exposes healthy brain tissue to radiation, potentially causing collateral, unintended damage. For the Mayo Clinic study, investigators used one of the most innovative and advanced forms of radiation treatment, called proton beam therapy. The cutting-edge, nonsurgical form of radiation therapy destroys cancer cells with targeted precision while minimizing side effects to surrounding healthy tissue.
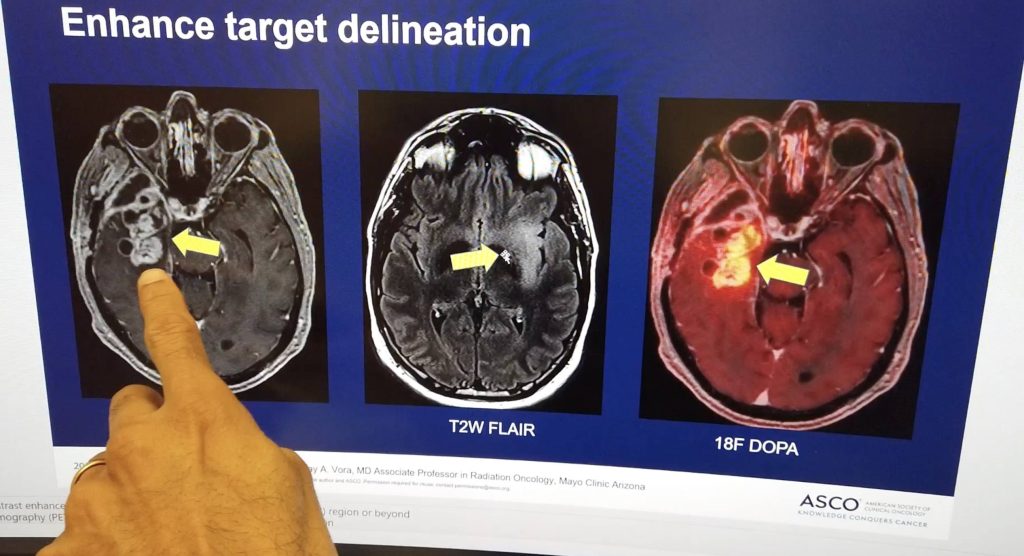
Mayo investigators mapped the target area in the patient's brain by combining the advanced imaging technologies, including 18F-DOPA PET and contrast-enhanced MRI. "Combining advanced imaging allowed us to determine the most metabolically active, or aggressive, regions of the glioblastoma," says Dr. Vora.
Treatment was completed in one to two weeks instead of the traditional three to six weeks. "The advanced imaging along with the proton beam therapy allowed us to be more focused with radiation and protect surrounding healthy brain tissue from the effects of radiation. We were able to see that patients tolerated the treatments well and lived longer than we expected."
According to Dr. Vora, the study at Mayo Clinic is the first clinical trial of its kind investigating the use of short-course hypofractionated proton beam therapy incorporating advanced imaging technology, including 18F-DOPA PET and contrast-enhanced MRI targeting, for patients 65 and older with newly diagnosed glioblastoma.
The study included patients from Arizona and Minnesota. One of the study participants, Richard Casper, lived nearly two years longer than his prognosis. "I feel great. If someone didn't tell me I had the glioblastoma, I wouldn't even know it," reported Casper after undergoing treatment. He succumbed to the disease in 2023. "We miss our dad dearly," says his daughter, Susan Casper. "We will forever be grateful for the extra time we had with our father. The time gave us a chance to make memories that will last us a lifetime. It was also important to my father to participate in this study in hopes of helping others fight glioblastoma."
A larger, randomized clinical trial is now underway at Mayo Clinic. One of the study participants is Nadya El-Afandi, a wife and mother of four, who lives in St. Paul, Minnesota. She was diagnosed with glioblastoma in 2022. El-Afandi is now 15 months post-treatment with no sign of glioblastoma. "I feel wonderful," says El-Afandi. "I've had my fourth MRI, and we're not seeing any return of the glioblastoma."
El-Afandi is back to her regular activities and just returned from a trip to Hawaii, where she spent time snorkeling and hiking. "We are living on the edge of medical miracles, and we are riding that tide. There's no cure for glioblastoma yet, but I've been able to take advantage of this medical opportunity, and it has given me a quality of life that is just outstanding," adds El-Afandi.
While El-Afandi's results are encouraging, William Breen, M.D., radiation oncologist and principal investigator of the current study says it is too early to draw any conclusions about the safety and efficacy of the treatment until the study is complete. "Our goal is to transform the way we treat glioblastoma using shorter courses of radiation to minimize the burden on patients and their families and help them complete safe and effective treatment in a shorter amount of time."
The clinical trial, known as SAGA, or stereotactic ablative radiation treatment for glioblastoma, includes patients from Arizona, Florida and Minnesota. "We are now adding another component that builds upon Dr. Vora's work to help us best visualize the tumor," says Dr. Breen.
Meanwhile El-Afandi is focusing on living her life to the fullest. "I'm so grateful," says El-Afandi. "Every day is the best day, and I'm going to enjoy every minute of it."
The study was funded by Mayo Clinic Marley Endowment Funds and the Lawrence W. and Marilyn W. Matteson Fund in Cancer Research. For a detailed list of the authors and disclosures, see the full paper here.






