Cervical cancer rates have declined, thanks to the Pap test and the Human Papillomavirus (HPV) vaccine, which can prevent 90% of cervical cancer.

However, disparities in cervical cancer outcomes persist among women of color, those with lower socioeconomic status and by geography. Medically underserved women account for more than 60% of current cervical cancer diagnoses.
UC Davis Comprehensive Cancer Center has launched the Healthy Cervix study, also called HEALIX, to determine the reasons for the prevalence of cervical cancer among those population groups. The research study is being conducted through a collaboration between the cancer center and Peach Tree Health, a Federally Qualified Health Center that operates clinics in Yuba, Butte, Sutter and Sacramento counties. The one-year research collaboration, launched in July 2024, will run until June 2025.
Seeking to reconcile disparities
HEALIX aims to reduce cervical cancer disparities among underrepresented and underserved women by increasing Pap and HPV testing as well as HPV vaccination among their adolescent children. The study will test new ways of encouraging and enabling women aged 21–65 to undergo cervical cancer screening. It will also examine new approaches to persuade parents to obtain HPV vaccinations for their children who are between the ages of 9 and 17.
The study will take place at three of Peach Tree's clinics in Yuba and Sutter counties. A fourth clinic, in Sacramento, will serve as the location for the control group. These participants will not receive screening and will serve as a baseline for assessing the effects of screening recruitment.
We need to understand if cultural stigmas and perhaps taboos regarding talking about sexual health are playing a role in low screening and vaccination rates."-Julie Dang, co-leader of HEALIX
Study basics
HEALIX study group leaders hope to enroll about 1,200 women and adolescents from diverse backgrounds in the study, primarily Spanish-speaking patients. In 2022, Peach Tree clinics in Live Oak, Yuba City and Marysville fell short of meeting screening and vaccination goals. HEALIX is exploring new approaches to increase rates at the same clinics.
"We need to understand if cultural stigmas and perhaps taboos regarding talking about sexual health are playing a role in low screening and vaccination rates," said Julie Dang, who is co-leading the HEALIX team with Laura Fejerman, associate director of the cancer center's Office of Community Outreach and Engagement. "We think the culturally tailored interventions we are testing may make a difference."
Peach Tree health educator Magali Cisneros is doing most of the outreach to test the new interventional approaches. She is following up at the clinics with Latina patients who have not been screened for cervical cancer or who canceled screening appointments.
"We are trying to reduce all the barriers that may be keeping these women from coming in for routine cervical cancer screenings, including speaking to them in their native Spanish language," Cisneros said.
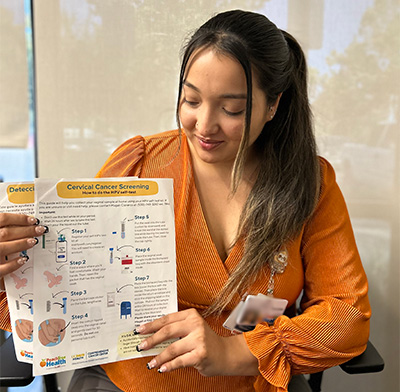
HEALIX is distributing $10 gas cards to study participants to cover their expenses to drive to a clinic. The study also offers either in-clinic cervical cancer testing or an HPV self-collection test, which can be done at the clinic or at home.
The U.S. Food and Drug Administration has approved the use of HPV tests that allow for self-collection in a health care facility. Researchers in the study are investigating whether women prefer using a self-test kit or in-clinic cervical cancer test. Everlywell, which manufactured the test kits for this study, created an IT clinic interface that is being used to register the kits and track results.
Pap vs. HPV tests
Until the mid-20th century, cervical cancer was commonly undetected in women until advancing to lethal stages, but the death rate fell after Pap tests became routine in the early 1960s.

The U.S. Preventative Services Task Force recommends screening for cervical cancer every three years with Pap tests alone in women aged 21 to 29 years. For women aged 30 to 65 years, it recommends screening every three years with Pap tests alone, every five 5 years with high-risk human papillomavirus (hrHPV) testing alone, or every five years with hrHPV testing in combination with Pap tests (co-testing).
Screen + vaccinate
"Once women get screened, either in clinic or at home, then we are giving them key prevention tips and letting them know about the HPV vaccine, which is best given to children between the ages of 9 and 12 and before they become sexually active," Cisneros said.
Dang added, "Basically, our goal is to convince moms of the importance of screening themselves and vaccinating their kids."







