A research team led by Professor Kelvin Yeung from the Department of Orthopaedics and Traumatology, School of Clinical Medicine, LKS Faculty of Medicine, the University of Hong Kong (HKUMed) has designed a new microneedle patch to offer a highly-effective non-antibiotic approach for the treatment of skin infection. In brief, the design engineered with ultrasound-responsive zinc-based metal-organic framework (MOF) antibacterial nanoparticles promises pain-free delivery to treat bacterial infection on skin tissue and facilitate skin repair at the same time. The novel microneedle is around 50 microns in diameter, similar to a typical hair. The findings have been published in Science Advances [link to publication].
Background
Acne is a common skin disease worldwide that upsets more than 80 % of teenagers and young adults.1 The primary cause can attribute to excessive lipid secretion that clogs the hair follicles, thereby establishing a hypoxic microenvironment in skin tissue. This undesirable condition particularly favours to the proliferation of Propionibacterium acnes (P. acnes) bacteria. Infected pimple, regarding as one of skin infections, is mainly caused by P. acnes bacteria that affects millions of people worldwide. It not only causes the patients with significant physical and emotional distress, but may also develop into chronic inflammatory condition without proper treatment. The clinical management normally includes non-prescription treatment (i.e., benzoyl peroxide and salicylic acid), or the administration of antibiotics orally or topically. However, such treatments can be ineffective or have unpleasant side effects.
In general, the first-line treatment for infected pimple is antibiotics administered either oral or topical. However, the therapeutic effect of topical antibiotic treatment is concerning, particularly when the drugs pass through the skin tissue. Also, the treatment becomes less effective, when bacteria are drug resistant or when they migrate to subcutaneous tissue. Especially, P. acnes bacteria can secrete extracellular polysaccharides to form biofilm that blocks out the attacks initiated by antibacterial agents or immune cells.
Even most microneedle products on the market mainly use pharmaceutical ingredients to treat acne. However, repeated applications of antibiotics may reduce the sensitivity of bacteria to drugs. Patients who have been affected by acne for a long time will know that the effects of the same treatment products can be significantly reduced after long-term use.
Research method and findings
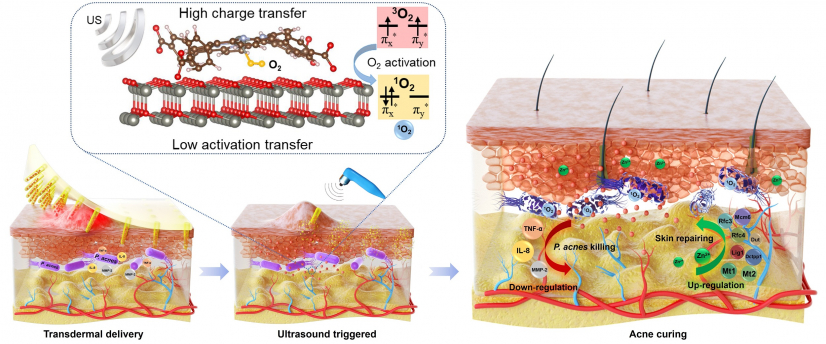
HKUMed team has invented a new microneedle patch that facilitates the transdermal delivery of ultrasound-responsive antibacterial nanoparticles to treat the infection induced by P. acnes at minimal invasive approach. In the current design, ultrasound-responsive antibacterial nanomaterials are introduced to the microneedle patch that responds to bacterial infection quickly and efficiently. The use of drugs is avoided in the treatment of acne. The modified nanoparticles comprised of ZnTCPP and ZnO are able to produce a substantial amount of reactive oxygen species (ROS) subject to ultrasound stimulation that can effectively oxidize the key cellular macromolecules of bacteria. The results demonstrate that the killing of P. acnes bacteria mediated by ROS can reach to 99.73% after 15 minutes of ultrasound stimulation. Also, the levels of inflammatory markers, including tumour necrosis factor-a (TNF-α), interleukins (ILs), and matrix metalloproteinases (MMPs) are significantly reduced. Furthermore, the zinc ions released can elevate the DNA replication-related genes, thereby augmenting more fibroblasts towards superior skin repair.
Research significance
Professor Kelvin Yeung Wai-kwok, remarked, 'The new microneedle patch enabling ROS generation upon ultrasound stimulation, regarding as a non-antibiotic and transdermal approach, can not only effectively address the infection induced by P. acnes bacteria, but also facilitates the skin repair due to zinc ion release. Due to the specific killing mechanism of ROS, we believe that this design is also able to address the other skin infections induced by fungi, parasites, or viruses, such as tinea pedis (namely "Athlete's Foot" or "Hong Kong Foot" in slang).'
About the research team
This research study was led by Professor Kelvin Yeung Wai-kwok, Department of Orthopaedics and Traumatology, School of Clinical Medicine, HKUMed. The first author Xiang Yiming is the PhD candidate under Professor Yeung's supervision. The research interests of Professor Yeung's team include orthopaedic biomaterials, musculoskeletal tissue regeneration and anti-bacterial infection.
Acknowledgements
This work was jointly supported by the National Key R&D Programmes of China (2018YFA0703100), the General Research Fund of Hong Kong Research Grants Council (Nos. 17207719 and 17214516), the Health Bureau Health and Medical Research Fund (Nos.19180712, 20190422 and 21200592), the Innovation and Technology Fund Partnership Research Programme (PRP/030/30FX), the National Science Fund for Distinguished Youth Scholars (No. 51925104), Shenzhen Science and Technology Programme (Nos. JSGG20180507183242702 and JCYJ20210324120009026), and the Shenzhen's Sanming Project of Medicine - 'Team of Excellence in Spinal Deformities and Spinal Degeneration' (SZSM201612055).