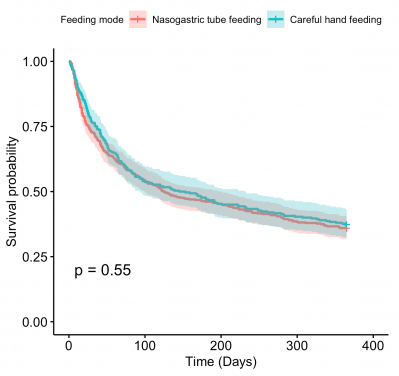
A HKUMed study found that there is little difference in one-year survival probability among advanced dementia patients on nasogastric tube feeding or careful hand feeding (125 days versus 145 days, Graph 1). But those on nasogastric tube feeding have a lower pneumonia-free survival probability compared with those on careful hand feeding (Graph 2).
A collaboration study led by researchers from the Division of Geriatrics, Department of Medicine, School of Clinical Medicine, LKS Faculty of Medicine at The University of Hong Kong (HKUMed) has found that advanced dementia patients with feeding problems initiated on careful hand feeding had a risk of pneumonia 40% lower than those on nasogastric tube feeding. The research article is now published online in the Journal of Post-Acute and Long-Term Care Medicine [link to the publication].
Background
Patients with advanced dementia with feeding problems such as poor oral intake and dysphagia are often initiated on tube feeding. Feeding tubes are inserted due to the perceived benefits of reducing the risk of aspiration pneumonia and improving survival. However, this has not been shown in previous observational studies conducted overseas.1 In recent years, some geriatric wards in Hong Kong have begun to offer the option of careful hand feeding as an alternative to tube feeding to promote comfort and quality of life in end-of-life patients with feeding problems.
The research team conducted the first study in Hong Kong of hospitalised patients with advanced dementia with feeding problems to compare the risk of pneumonia and death between those initiated on careful hand feeding versus nasogastric tube feeding.
Research findings
The retrospective cohort study identified 764 patients with advanced dementia considered for tube feeding due to feeding problems.2 The findings showed that patients initiated on careful hand feeding had a risk of pneumonia 40% lower than those on nasogastric tube feeding.
There was no significant difference in one-year survival between the nasogastric tube feeding and careful hand feeding groups, with a median survival of 125 and 145 days respectively.
Research significance
This study provides evidence that, contrary to conventional wisdom, nasogastric tube feeding does not confer survival benefits compared with careful hand feeding in patients with advanced dementia. Moreover, nasogastric tube feeding is associated with an increased risk of pneumonia compared with careful hand feeding in this patient population. Postulated mechanisms for increased aspiration risk with nasogastric tube feeding include impairment of the lower oesophageal sphincter, desensitisation of the pharyngoglottal reflex, and reflux of gastric contents into the pharynx.3
'As the practice of tube feeding in advanced dementia patients remains prevalent in Hong Kong and many parts of the world, this research highlights the need for further education of the public and healthcare providers to improve evidence-based practice around tube feeding decisions in dementia patients,' commented Dr Jacqueline Yuen Kwan-yuk, Clinical Assistant Professor of the Division of Geriatrics, Department of Medicine, School of Clinical Medicine, HKUMed.
About the research team
The research was conducted by Dr Jacqueline Yuen Kwan-yuk, Dr James Luk Ka-hay, Dr Ivan Chan Tuen-ching, Dr Shea Yat-fung and Professor Felix Chan Hon-wai, Division of Geriatrics, Department of Medicine, School of Clinical Medicine, HKUMed, and TWGHs Fung Yiu King Hospital. Other collaborators include Steven Chu Tsun-wai, Student Research Assistant, Division of Geriatrics, Department of Medicine, School of Clinical Medicine, HKUMed; Dr Rachelle Bernacki, Department of Psychosocial Oncology and Palliative Care, Harvard Medical School; and David Chow Tak-yu, Department of Speech Therapy, TWGHs Fung Yiu King Hospital and Grantham Hospital.
Acknowledgements
This study was supported by the University Research Committee of The University of Hong Kong (201904185003).






