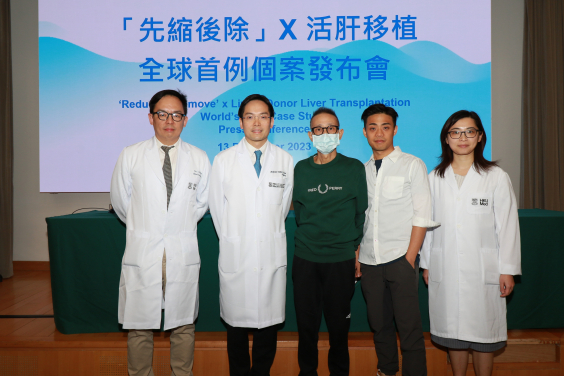
The HKU liver cancer research team achieves a groundbreaking milestone with the 'Reduce and Remove' approach, successfully curing stage 4 liver cancer by 'reducing' it to an early stage 1 tumour and then 'removing' it by living donor liver transplantation. This is believed to be the first reported case of its kind worldwide, representing a breakthrough in liver cancer treatment. (From left: Dr Chiang Chi-leung, Clinical Assistant Professor, Department of Clinical Oncology, Centre of Cancer Medicine, School of Clinical Medicine, HKUMed; Professor Albert Chan Chi-yan, Clinical Professor, Department of Surgery, School of Clinical Medicine, HKUMed; patient Mr Wong and his son; Dr Chan Miu-yee, Honorary Clinical Assistant Professor, Department of Surgery, School of Clinical Medicine, HKUMed.)
A new treatment strategy for locally advanced liver cancer, known as 'Reduce and Remove', was announced by the Department of Surgery and Department of Clinical Oncology, Centre of Cancer Medicine, School of Clinical Medicine, LKS Faculty of Medicine of the University of Hong Kong (HKUMed) earlier this year. This innovative approach provides a way for patients with inoperable locally advanced liver cancer to be cured. One remarkable case among patients treated with the 'Reduce and Remove' strategy involved the conversion of stage 4 liver cancer to stage 1 cancer, followed by the removal of the tumour through living donor liver transplantation. This novel treatment was also used for a second patient of advanced age who subsequently underwent this liver-preserving surgery. The liver transplantation case was presented at the Congress of the Asian Society of Transplantation 2023 and was recently published in Liver Cancer [Link to the publication].
Background
Liver cancer ranks as the fifth most common cancer in Hong Kong1, with over 1,700 new cases per year. Previously, liver surgery and liver transplants were the only curative treatments available. However, only 30% of the patients are amenable to these treatment options, leaving the remaining 70% of patients with a five-year overall survival rate of only approximately 30%. Hence, extensive research efforts are devoted to expanding the role of surgery or transplantation for this deadly disease, where possible.
Patient cases
Led by Professor Albert Chan Chi-yan, Clinical Professor, from the Department of Surgery, School of Clinical Medicine, and Dr Chiang Chi-leung, Clinical Assistant Professor, from the Department of Clinical Oncology, Centre of Cancer Medicine, School of Clinical Medicine, HKUMed, the HKU liver cancer research team has pioneered the 'Reduce and Remove' approach, using a combination strategy of stereotactic body radiation (SBRT) and immunotherapy (IO) to induce shrinkage of locally advanced liver cancer. For the first time in the world, Professor Chan and his team successfully cured stage 4 liver cancer by 'reducing' it to an early stage 1 tumour with this combination strategy and then 'removing' it by living donor liver transplantation. The research team used the same strategy for an 85-year-old patient with two liver cancers, the most senior patient to date, and then successfully removed the tumour by liver-preserving surgery.
The first patient, Mr Wong (aged 65), who had hepatitis B, presented with abdominal distension in November 2022. Computed tomography showed a liver tumour 18.2cm in diameter, covering the left side of his liver with main portal vein invasion (stage 4). Mr Wong's tumour marker, AFP, was over 100,000ng/ml upon presentation, his life expectancy was about six months. Given Mr Wong's advanced stage of disease, the liver cancer research team started the novel 'Reduce and Remove' strategy. Over the following six months, Mr Wong's tumour size gradually decreased from the initial 18.2cm to 9cm on subsequent scans and his AFP level dropped to 80ng/ml. To achieve a complete cure, liver transplantation was the only feasible option, and his son volunteered to be the donor. The living donor liver transplantation involved two teams of surgeons. The operation was performed on 21 August 2023 and took 12 hours. The operation was successful, and Mr Wong was discharged from hospital 15 days after his operation. Post-operative liver function was normal, and his AFP level remained at 2ng/ml in the three months after the transplantation. The final analysis of the liver revealed only a 1.5cm tumour (stage 1) remaining viable; no other tumours were found in the rest of the liver. Mr Wong has remained well and cancer-free for nearly four months since the operation. This is believed to be the first reported case in the world.
The second patient, Mr Got (aged 85), with hypertension, diabetes and pulmonary tuberculosis, was found to have two liver cancers – one in the right side of the liver (6.5cm in diameter) and the other in the left side (3.1cm in diameter), which compressed left hepatic vein. Considering Mr Got's age, the surgical risk was very high. After receiving the combination 'Reduce and Remove' treatment, the active component of Mr Got's tumours shrank to 2.3cm and 1.8cm, respectively. Professor Chan and his surgical team then successfully performed a parenchymal preserving liver surgery to remove both tumours. Mr Got recovered well and was discharged from hospital four days after the operation.
Research significance
'The team is honoured to provide new hope and possibilities for the treatment of liver cancer, curing the patient by converting stage 4 liver cancer to stage 1 cancer, and then removing the tumour by living donor liver transplantation, which is believed to be the first such case in the world. The recovery progress of the patient is encouraging,' said Professor Albert Chan Chi-yan, Clinical Professor, the Department of Surgery, School of Clinical Medicine, HKUMed.
The team's innovative 'Reduce and Remove' treatment strategy has profound research significance and clinical value for liver cancer patients and the medical community. 'The HKU-pioneered "Reduce and Remove" strategy is a breakthrough in liver cancer treatment,' Professor Chan further explained, 'This strategy effectively prolongs the lives of patients, especially patients for whom the tumour stage and size must be reduced before liver transplantation. Moreover, this strategy involves low invasiveness, and it is safe and well-tolerated, even in elderly patients, who are normally not suitable for high-risk and complex surgery.'
This treatment strategy provides a definite treatment schedule. Most patients can have an idea of the treatment effect within six months after the start of treatment, allowing better planning for themselves and their families. The team is looking forward to seeing this new strategy result in a new direction of treatment for the world, inspiring more research, innovation, communication and collaboration, and benefiting more liver cancer patients.
About the research team
The study is led by Professor Albert Chan Chi-yan, Clinical Professor, Department of Surgery, and Dr Chiang Chi-leung, Clinical Assistant Professor, Department of Clinical Oncology, Centre of Cancer Medicine, School of Clinical Medicine, HKUMed.






