Scientists at EPFL have uncovered a cunning strategy that SARS-CoV-2, the virus that causes COVID-19, uses to increase its infectivity.
SARS-CoV-2, the novel coronavirus first identified in late 2019, has since spread globally, leading to the COVID-19 pandemic that has affected millions. As countries grapple with its health, social, and economic impacts, scientists and researchers worldwide have been working tirelessly to understand the virus better and develop effective treatments and vaccines.
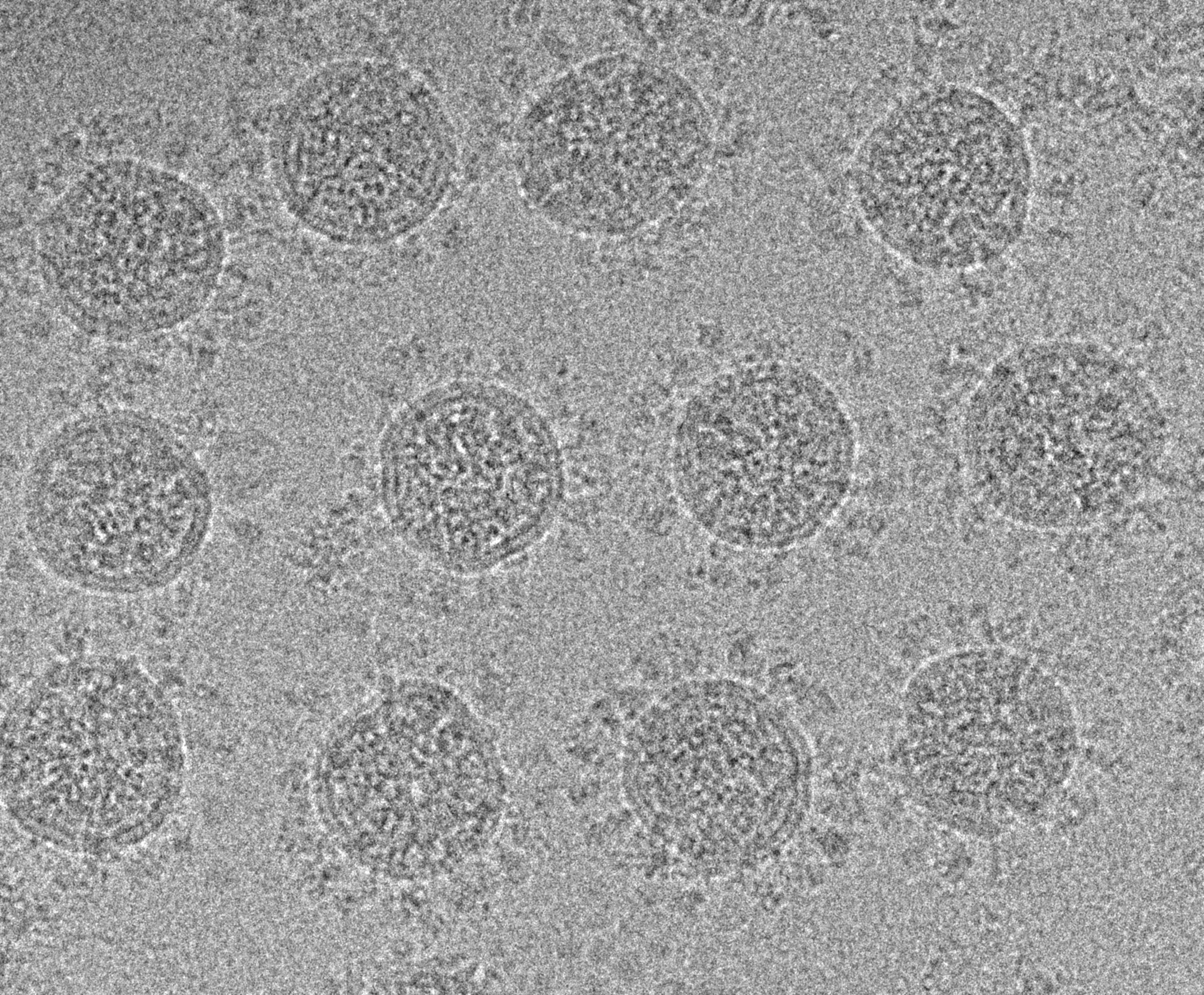
In a new study, researchers at EPFL have unveiled a novel mechanism by which SARS-CoV-2 increases its infectivity. The study focuses on the virus's notorious Spike protein, which allows it to enter and infect human cells.
The research, now published in Nature Communications, was led by Francisco S. Mesquita and Laurence Abrami in the group of Gisou van der Goot at EPFL's School of Life Sciences.
Upon infecting a host, SARS-CoV-2 manipulates its cellular machinery to modify an enzyme that then turbocharges Spike's ability to invade other cells. The enzyme, abbreviated as ZDHHC20, normally tags proteins with a little fat molecule that changes the way they work.
But upon infection, the virus takes over the ZDHHC20 enzyme. "In our previous work, we discovered the enzyme that modifies the SARS-CoV-2 Spike protein - it adds lipids to it - and this is essential for the virus to fuse with target cells," says Gisou van der Goot. "What we now show is that the virus actually triggers an optimization of the enzyme by inducing a change in the transcription of its gene."
Analyzing the effects of SARS-CoV-2 on the gene (zdhhc20), the researchers found that the virus triggers a change in its transcriptional start site - the part of a gene where the process of "reading" it into a protein begins.
Studying both cells in the lab and live organisms, they confirmed that this "transcriptional change" produces an enzyme with 67 additional amino acids. This is enough to increase its lipid-adding activity on Spike 37 times, leading to a heavily enhanced viral infectivity.
The team also used metabolic labeling, Western blotting, and immunofluorescence to visualize and quantify proteins, and get a comprehensive view of the virus's manipulative tactics.
Digging deeper, the researchers found that this change in the transcriptional start of genes seems to be something cells normally do in response to stresses or challenges - in the case of the study, chemically-induced colitis. What this means is that SARS-CoV-2 hijacks a pre-existing cell damage response pathway to generate more infectious viruses.
The discovery highlights SARS-CoV-2's tactics to boost its infectivity, offering a blueprint for potential treatments, and suggests that other viruses might use similar strategies of co-opting host defenses. Additionally, the findings indicate that the cellular response the virus leverages could be a general reaction to various stresses, which expands the study's findings beyond viral infection.






