Obesity, diabetes and gastrointestinal cancer are frequently linked to an unhealthy diet. However, the molecular mechanisms responsible for this are not fully understood. Researchers at the Technical University of Munich and Helmholtz Munich have gained some new insights that help to better understand this connection. These findings provide an important basis for the development of new, non-invasive therapies.
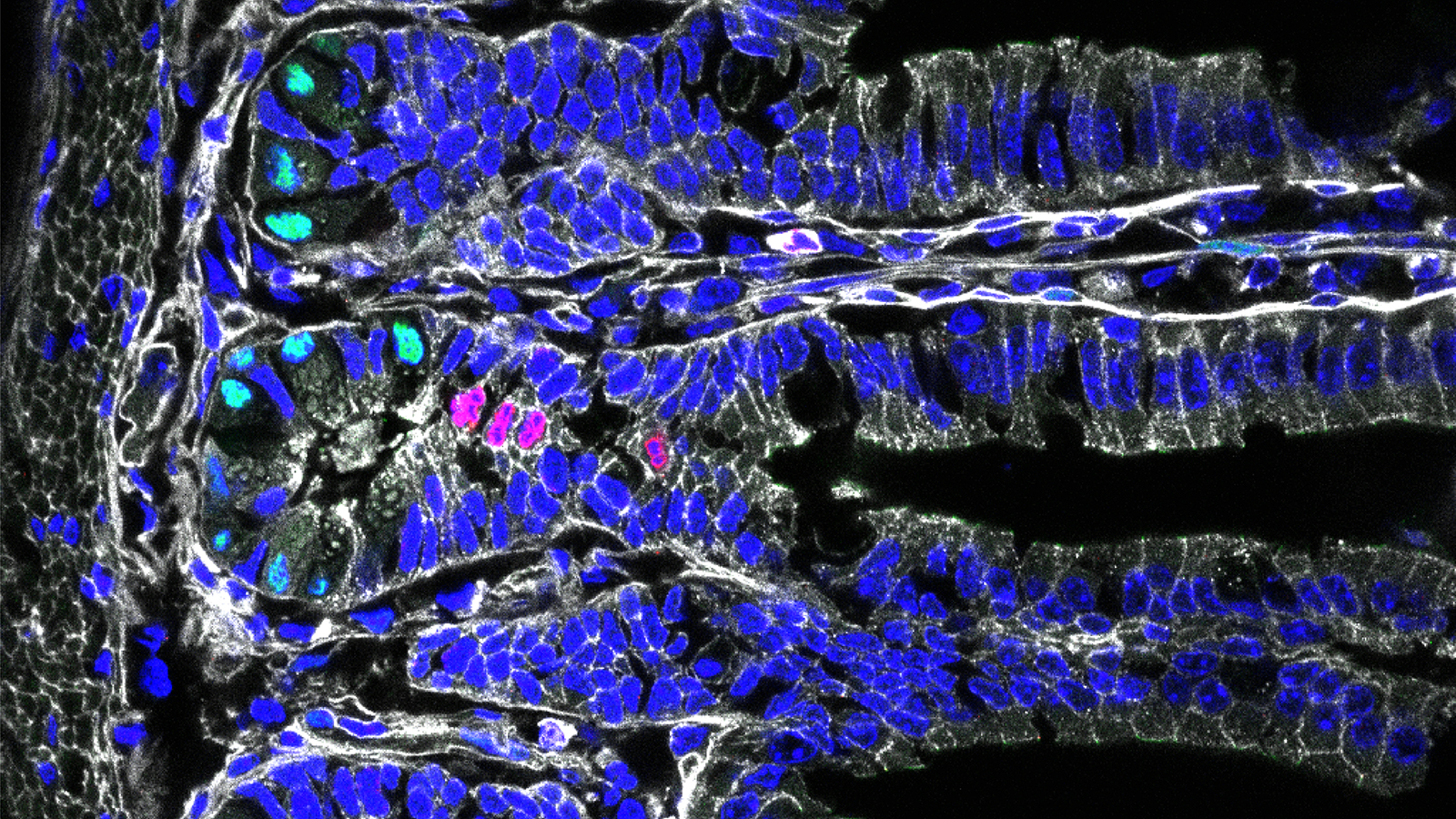
The intestine is essential for maintaining our energy balance and is a master at reacting quickly to changes in nutrition and nutrient balance. It manages to do this with the help of intestinal cells that among other things are specialized in the absorption of food components or the secretion of hormones.
In adult humans, the intestinal cells regenerate every five to seven days. The ability to constantly renew and develop all types of intestinal cells from intestinal stem cells is crucial for the natural adaptability of the digestive system. However, a long-term diet high in sugar and fat disrupts this adaptation and can contribute to the development of obesity, type 2 diabetes and gastrointestinal cancer.
Important role of the intestinal stem cells
The molecular mechanisms behind this maladaptation are part of the research field of the group of Heiko Lickert, professor for diabetes research and ß-cell biology at the Technical University of Munich and head of the Institute for Diabetes and Regeneration Research at Helmholtz Munich.
The scientists assume that intestinal stem cells play a special role in the maladaptation. Using a mouse model, the researchers investigated the effects of a high-sugar and high-fat diet and compared it with a control group.
Important basic research for non-invasive therapies
These and other findings from the study lead to a new understanding of disease mechanisms associated with a high-calorie diet. "What we have found out is of crucial importance for developing alternative non-invasive therapies," says study leader Heiko Lickert, in summarizing the results.
To date, there is no pharmacological approach to prevent, stop or reverse obesity and diabetes. Only bariatric surgery causes permanent weight loss and can even lead to remission of diabetes. However, these surgeries are invasive, non-reversible and costly to the healthcare system.
Novel non-invasive therapies could happen, for example, at the hormonal level through targeted regulation of serotonin levels. The research group will examine this and other approaches in subsequent studies.
(Kopie 4)
Publications:
Alexandra Aliluev, Sophie Tritschler, Michael Sterr, Lena Oppenländer, Julia Hinterdobler, Tobias Greisle, Martin Irmler, Johannes Beckers, Na Sun, Axel Walch, Kerstin Stemmer, Alida Kindt, Jan Krumsiek, Matthias H. Tschöp, Malte D. Luecken, Fabian J. Theis, Heiko Lickert and Anika Böttcher
Diet-induced alteration of intestinal stem cell function underlies obesity and prediabetes in mice
Nature Metabolism vol. 3, pages 1202-1216 (2021) - DOI: 10.1038/s42255-021-00458-9






