For over a decade, Columbia geneticist Angela Christiano, PhD, has attended the annual meeting of the National Alopecia Areata Foundation, where hundreds of individuals affected by the hair loss disorder gather to support one another and learn about the latest scientific research. The meeting is a safe space where patients with alopecia, many of whom have lost all their hair, joyfully remove their wigs and head coverings for the three-day celebration, without fear of shame or judgment.
But this year's meeting was a bit different. Christiano had trouble recognizing conference attendees she's known and worked with for years, because many of them now have full heads of hair.
For people with alopecia areata, an autoimmune disease that can cause hair loss so complete that people even lose their eyebrows, the change in appearance was dramatic.
It was also a direct result of Christiano's groundbreaking research on the condition, which led the FDA in June to approve the first systemic treatment specifically developed for severe alopecia areata.
"It's a strange feeling. It's what every geneticist dreams of, to find the genes for a condition and develop a treatment that can directly benefit patients. But it's extremely rare that it actually works out that way," says Christiano, who has studied alopecia areata for more than 20 years, motivated by her own bout with the disease.
Mysterious origins
Unlike hormone-driven male pattern baldness, alopecia areata is an autoimmune disease in which the body's own immune system mistakenly attacks the hair follicle and shuts down hair production.
When Christiano began working on it, though, nobody knew exactly what caused the problem.
Starting with a series of basic research studies on the genetics and cell biology of hair growth, Christiano and a multidisciplinary team of collaborators produced a steady stream of advances, first in the lab and then in the clinic.
The first major clue came in 2010, from a study led by Christiano's team that looked through the genomes of a thousand patients. The study, published in Nature, uncovered a gene that, when abnormally expressed, produces a known "danger signal" that causes the body to recognize the hair follicle as foreign.
The genome study was also crucial since the findings also explained why previous efforts to treat the condition hadn't worked.
"Drugs for other autoimmune skin diseases had been tested in alopecia, but they had largely failed," Christiano says.
"At that point, we realized that was because alopecia doesn't share genetic pathways with other autoimmune skin diseases."
Taming killer T cells
The genome study led the team to focus on investigating a particular kind of "killer" T cell recruited by the danger signal, which became central to understanding the mechanism of hair follicle destruction.

Christiano is not an immunologist, so she needed to enlist an expert to help make inroads into understanding the behavior of these cells. She approached Raphael Clynes, MD, PhD, at that time a faculty member in the Department of Medicine, who was an expert in studying the same kinds of killer T cells in type 1 diabetes and in cancer.
Clynes looked at the list of genes from the genome study and images of the "swarm" of killer T cells surrounding the hair follicle and suggested that inhibiting enzymes known as JAK kinases might be one way to treat the disease.
The team showed that small molecule drugs called JAK inhibitors could shut down signaling inside the killer T cells. Amazingly, by inhibiting the JAK pathway, the team found they could reverse alopecia areata in a mouse model of the disease.
Dramatic regrowth of hair
Armed with photos of mice with alopecia that had regrown all their hair, Christiano next approached her colleague Julian Mackay-Wiggan, MD, a Columbia dermatologist who specialized in hair disorders and had an interest in early-stage clinical research.
Excited by the early results in the mice, Mackay-Wiggan began treating a few patients with alopecia areata using JAK inhibitors that were already FDA-approved for other disorders. The first few patients experienced dramatic regrowth of their hair, just as the researchers had observed in the mice. Christiano's team reported these groundbreaking studies in 2014.
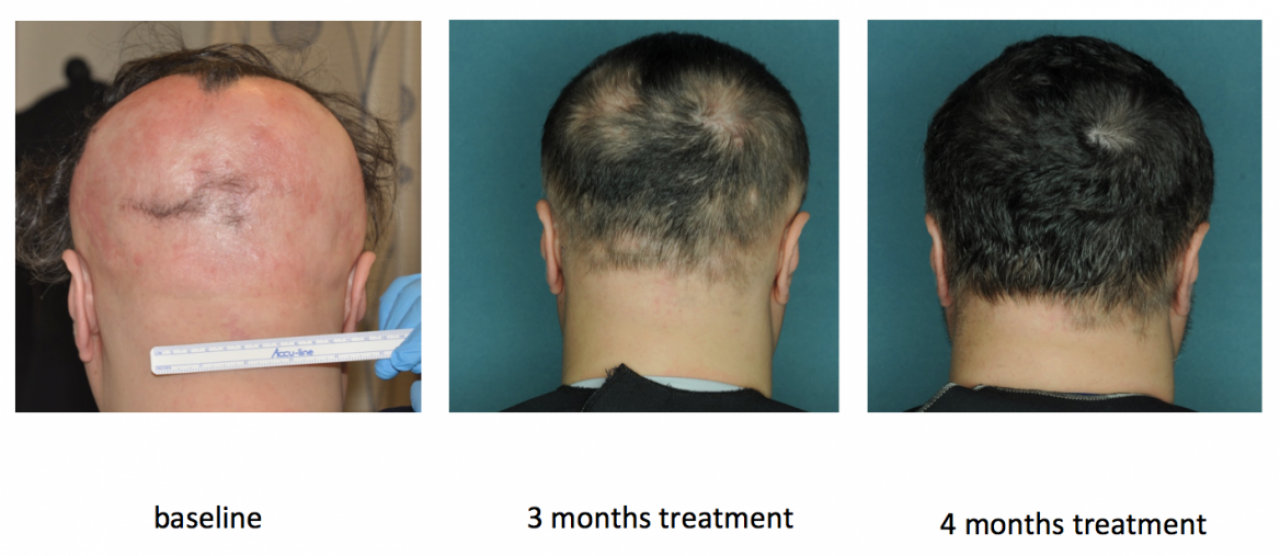
Building on these early results, Mackay-Wiggan conducted additional Columbia clinical studies that showed that 75% of patients experienced significant hair regrowth after treatment with two different JAK inhibitors.
Pharma attention
Soon after the Columbia team reported its findings, additional case reports began appearing in the published literature that replicated the results in alopecia patients from around the world.
Because there were no FDA-approved drugs for alopecia when their work began, it didn't take long for pharmaceutical companies to turn their attention to developing JAK inhibitors specifically for alopecia treatment. These efforts led to newly approved Olumiant from Eli Lilly, Incyte (previously approved for rheumatoid arthritis and hospitalized patients with COVID-19), and two additional JAK inhibitors being developed by Pfizer and Concert Pharmaceuticals and now in late-stage clinical trials.
"The impact of this treatment on patients has been truly transformative."
Christiano welcomes the pharmaceutical companies' new attention to alopecia areata after the condition had long been neglected and was frequently dismissed as a cosmetic problem.
For patients with complete hair loss, the barrage of stares and intrusive questions can be demoralizing and psychologically devastating. "It's the stigma of unwanted attention; how do you quantify that?" says Christiano. "The impact of this treatment on patients has been truly transformative."
Male pattern baldness next?
While Olumiant and other new JAK inhibitors are often life-changing for patients who respond well to them, the treatments are still far from perfect.
"These are potent immunosuppressive drugs, so there are safety considerations to be taken into account when assessing the risk/benefit ratio for individual patients," says Christiano. After the treatment ends, some patients' alopecia relapses for reasons the researchers don't fully understand. In addition, about a third of patients don't respond to the drugs.
Fortunately, Christiano has no intention of resting on her laurels. Her lab is hoping to understand what causes the condition to relapse after JAK inhibitor treatment.
And by continuing to investigate alopecia areata with new tools and techniques, her team is developing both new biological insights and more potential ways to attack the disease process. "We're now looking upstream of the JAK signaling pathway to see if other mechanisms can lead to the common endpoint of alopecia areata," she says.
Christiano's team also hopes to extend these insights and apply the same approaches to treat other types of hair loss.
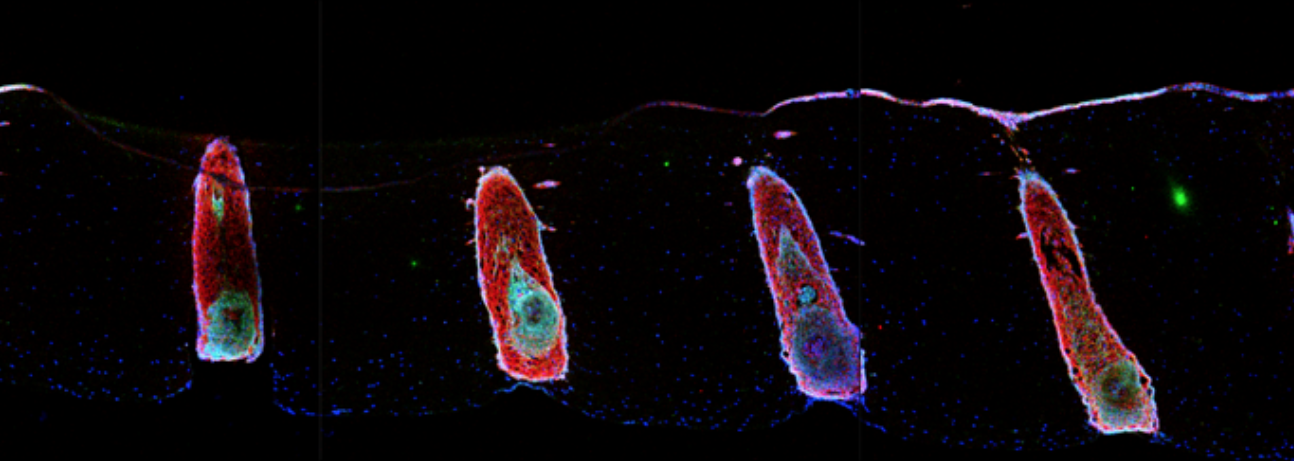
In one recent study, for example, Christiano's team found that JAK inhibitors also reawaken dormant hair follicles, a problem common to male and female pattern baldness.
They also discovered a previously unknown type of immune cell that puts hair follicles into a dormant state by secreting a substance called oncostatin M and that the hair cycle can be reactivated by blocking this pathway.
While translating these results into effective treatments for hair loss will likely take years, it's a process Christiano now knows well.
References
More information
Angela M. Christiano, PhD, is the Richard and Mildred Rhodebeck Professor of Dermatology, vice chair of research in the Department of Dermatology, and professor of genetics & development at Columbia University Vagelos College of Physicians and Surgeons. She also serves as an Advisory Dean for Basic Science Faculty. In 2020, Christiano was elected to the National Academy of Sciences.
Raphael Clynes, MD, PhD is currently vice president of translational biology at Xencor Inc.
Julian Mackay-Wiggan, MD, MPH, is currently in practice in the Siperstein Dermatology Group.






