A "lab-grown model" of the human stomach that can be used to study how infections impact the gastrointestinal system, has been developed for the first time by a UCL-led team of international scientists.
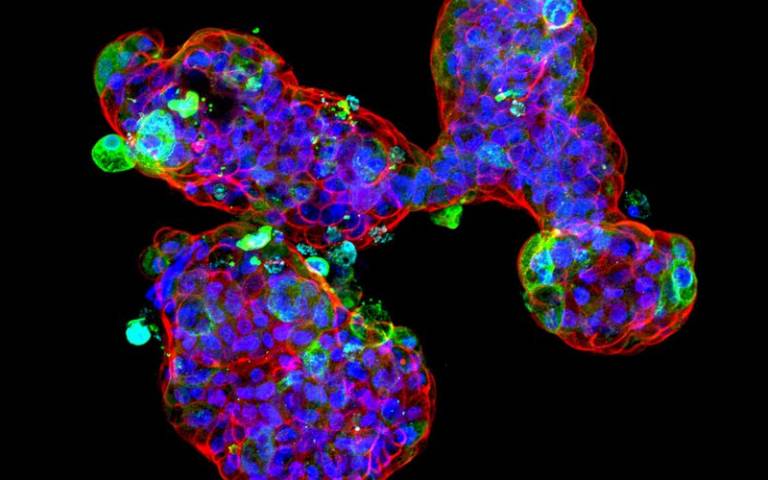
The team from Great Ormond Street Hospital (GOSH), UCL Great Ormond Street Institute of Child Health (UCL GOS ICH) and the Istituto Zooprofilattico Sperimentale delle Venezie (Legnaro, Italy), have built on recent advances to grow 'mini-organs' in a laboratory, known as organoids. These organoids provide researchers with invaluable tools to study how organs function both when they are healthy and when impacted by disease.
In this study, published in Nature Communications, scientists have for the first time described how to grow mini-stomach organoids, across differing stages of development - fetal, child and adult.
To do this, researchers, based at Zayed Centre for Research into Rare Disease in Children, isolated stem cells from patient stomach samples, and grew them under special conditions in the lab to obtain mini-stomachs in a dish that mimic the behaviour of a human stomach.
As the COVID-19 pandemic progressed, several hospitals reported gastrointestinal symptoms alongside the more usual respiratory effects like coughs and breathing difficulties, particularly in children. Following these cases, the research team, led by Dr Giovanni Giuseppe Giobbe, Professor Nicola Elvassore and Professor Paolo De Coppi from UCL GOS ICH, and Dr Francesco Bonfante from Istituto Zooprofilattico Sperimentale delle Venezie, determined that their mini-stomach model could be used to study how a SARS-CoV-2 infection affects the stomach.
The scientists were able to facilitate the infection of the mini-stomachs from the outside by exposing the surface of the cells to the virus. From this they showed that SARS-CoV-2 could replicate within the stomach, more noticeably in organoids that were grown from the child and late fetal cells, compared to adult and early fetal cells.
The research team were also able to look at the impact of the infection on the cells within the organoids, showing that a specific group of cells, called delta cells that make a hormone called somatostatin, had died, which could explain some of the stomach symptoms seen in patients. The team's laboratory results mirror the pattern of gastrointestinal symptoms seen in patients of different ages.
Professor Paolo De Coppi, (GOSH Consultant Paediatric Surgeon and UCL GOS ICH Nuffield Professor of Paediatric Surgery), senior author said: "This study has highlighted that SARS-CoV-2 infection may begin to infect the gastrointestinal system via the stomach in children and young babies. We hope that this adds another piece to the puzzle as we try to build our understanding of the impact of the virus across the body. As a research team we are proud to have been able contribute to the global fight against coronavirus in this way, pivoting our research as the need arose."
The team now plan to continue their work utilising these new mini-stomachs, aiming to study how the stomach develops from early in pregnancy through to adulthood. They also hope to look at the effects of other common gastrointestinal infections.
Dr Giovanni G Giobbe (UCL GOS ICH Senior Research Associate) and co-lead author on the study said: "We have been able to develop the first fetal model of the stomach and have demonstrated that the human gastric organoids can be used to accurately study real-world infections. Developing reliable models of organs that scientists and doctors can study in a lab are vital as they allow us to work out how organ tissue is affected during disease and infection. We want to increase our understanding of how infections impact the stomach so that we can further the search for new treatments."






