Researchers at the University of Toronto's Institute of Biomedical Engineering have found that studying blood flow in leg muscles may help detect cardiovascular disease earlier than standardized tests, opening the door to earlier treatment and better outcomes.
While medical imaging has improved the ability to find heart-specific issues, such as stiffening or scarring of heart tissue, these tests typically miss even earlier signs of trouble in other parts of the body.
Indeed, previous research suggests that poor blood flow regulation in leg muscle may show up before similar changes in the heart, and could even explain symptoms like fatigue or difficulty exercising.
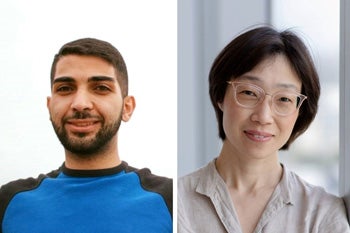
"Our study shines a light on an important gap in how we detect HFpEF before the heart becomes irreversibly damaged," says Hai-Ling Margaret Cheng, a professor at the Institute of Biomedical Engineering and senior researcher on the project.
HFpEF, or heart failure with preserved ejection fraction, is a common and challenging condition that affects millions of people worldwide. It progresses quietly and shows few symptoms until it becomes serious and difficult to treat.
"Our work suggests that vascular changes in leg muscle could serve as an earlier, more accessible warning sign of the disease."
To explore this idea, the research team - whose work was published in the journal Discover Medicine - used a special type of MRI scan that tracks how blood vessels respond to stress. They tested this method in a preclinical model of diabetes-induced HFpEF, focusing on blood flow changes in both the heart and the leg muscle. They found that in diabetic subjects, problems in blood flow regulation in the leg muscle appeared months before similar issues were seen in the heart. This suggests that leg muscle may offer a better location to catch HFpEF in its early stages.
"Our results show that by looking at blood flow in the legs, we could detect problems much sooner than we would by focusing only on the heart," says the study's lead researcher Sadi Loai, who completed his PhD in biomedical engineering at U of T.
"This could make a big difference in how we diagnose and treat this condition."
Looking ahead, Cheng emphasized the next steps for the research.
"The next step is to test human patients with the risk factors for HFpEF and determine if our MRI platform can, indeed, identify disease earlier than can conventional diagnostic methods," she says.
"Our ultimate goal is not only to open a door to early diagnosis when this disease may be treatable, but also to offer a new direction in treating a condition that is growing in prevalence and has become the most common form of heart failure."






