In the past, people with lymphoedema were advised to go to great lengths to protect the affected limb, but a growing body of research indicates that this is not always necessary.
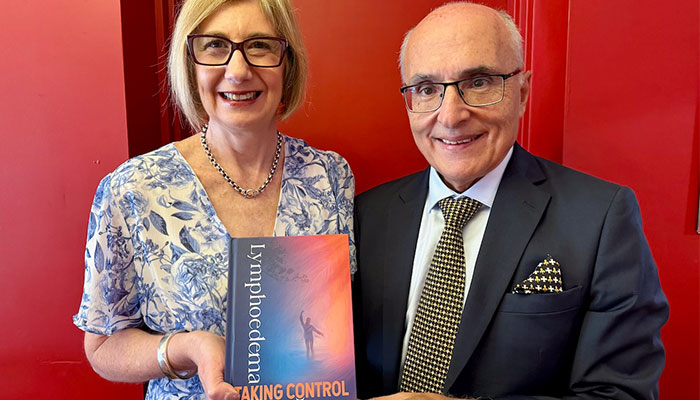
Mythbusters: Expert authors Associate Professor Louise Koelmeyer, left, and Professor John Boyages AM, right, give patients the latest research findings and management advice in their new book, Lymphoedema: Taking Control.
Living with the condition or being at risk of developing it does not mean avoiding everyday activities or necessary medical procedures.
By understanding the latest guidelines and following sensible precautions, people with lymphoedema can lead active, healthy lives without worrying about worsening their condition.
What is lymphoedema?
Lymphoedema results in the accumulation of lymphatic fluid in the tissue, usually in one or more limbs. This swelling can be painful and disfiguring. If left untreated, it can be irreversible.
About one in five breast cancer patients who have had lymph nodes surgically removed or irradiated as part of their treatment goes on to develop the condition.
Like blood plasma, lymphatic fluid circulates the body's lymphatic system, carrying white blood cells and nutrients, collecting debris and harmful substances, and fighting infection.
The fluid can leak from blood vessels into the surrounding tissue, but usually, the lymph nodes in the armpits and on both sides of the groin drain it away. If any of these are lost, it can affect the functioning of this drainage system.
Over the past 10 years, the advice for treating and managing lymphoedema has been updated dramatically, thanks to research carried out at the Australian Lymphoedema Education, Research and Treatment (ALERT) Centre at Macquarie University.
Busting the myths
Myth: Losing lymph nodes means you will develop lymphoedema
Fact: Not everyone who loses lymph nodes will go on to develop lymphoedema, and patients' risk can be assessed with reasonable accuracy. For example, someone who has had one sentinel lymph node removed, has not had chemotherapy or radiotherapy, and is not overweight has a risk of less than 5 per cent. Even for people at increased risk, the latest monitoring techniques, such as bioimpedance spectroscopy and indocyanine green lymphography, mean the condition can be caught in its very early stages and any swelling controlled or prevented altogether.
Myth: Lymphoedema patients should avoid exercise
Fact: Exercise, including going to the gym and lifting weights, is safe and beneficial for individuals with lymphoedema. Research has demonstrated that progressive strength training improves strength, physical function, and quality of life without worsening lymphoedema. In a recent study, we found that being overweight increased the risk of developing lymphoedema.
We also found that people with the condition gained more weight, so keeping fit is doubly important. However, you should start slowly and increase intensity gradually, ideally under the guidance of a personal trainer or exercise physiologist.
Myth: Flying can cause lymphoedema
Fact: The belief that air travel can cause or worsen lymphoedema is largely unfounded. Research, including the PREVENT Study done by ALERT with Vanderbilt University in the United States of America, has shown no significant link between flying and the development of lymphoedema, particularly for people who have had only one sentinel node removed.
People with confirmed lymphoedema should wear a compression garment during long flights, and people who are at high risk (for example, those who have had a complete axillary dissection (clearance) with radiation) should consider following suit. Compression is not necessary for short flights. Staying hydrated and moving regularly during the flight are simple yet effective ways to maintain circulation.
Myth: Injections and medical procedures should be avoided in the affected arm
Fact: The risk of developing lymphoedema from a simple blood test or medical procedure is extremely low. Using the unaffected arm for injections and blood tests is preferable, but it may not always be possible. If the affected arm must be used, ensure the procedure is performed carefully and cleanly to prevent cellulitis. Monitor the arm afterwards for any sign of infection, such as redness or warmth.
The risk of harm from vaccinations is also low, but it is recommended that vaccines should be administered in an unaffected arm or leg unless there is no other option.
Myth: Blood pressure should not be taken on the affected arm
Fact: Taking blood pressure on an arm affected by lymphoedema is generally safe and unlikely to cause harm, though it is preferable to use the unaffected arm if possible as it can cause discomfort. Manual blood pressure devices are recommended over automatic ones, as they allow for controlled cuff inflation, reducing the risk of excessive pressure.
Myth: Outdoor activities like going to the beach or gardening should be avoided
Fact: Both activities are safe for people with lymphoedema, provided they take standard precautions to protect themselves from the sun, minor injuries, and insect bites. Using sunscreen, wearing protective clothing, and staying hydrated are key in preventing sunburn and minimising the risk of aggravating lymphoedema symptoms. Bad sunburn can also increase the risk of cellulitis. For gardeners, the advice is the same for people with or without lymphoedema: wear properly fitting gloves, protective clothing and insect repellent to protect against injuries and bites that may lead to infections.
Myth: Early detection of lymphoedema is not necessary
Fact: It's not enough to follow up with patients and wait for visible swelling to occur. By detecting lymphedema months or even years earlier, we can intervene sooner and, in many cases, prevent its progression.
In the PREVENT study, investigators from Macquarie and Vanderbilt University showed that early detection of lymphedema using bioimpedance devices (such as the SOZO) significantly reduced the risk of chronic lymphedema by 59 per cent compared to the old-fashioned tape measure.
About one in five patients who developed subclinical lymphedema detected by tape measure progressed to chronic lymphedema compared to one in 13 patients detected by bioimpedance.
Lymphoedema: Taking Control, published by BC Publishing, is a guide for patients, caregivers, lymphoedema therapists and other health professionals.
Professor John Boyages, AM is a Professor of Breast Oncology and the Founding Director of ALERT.
Associate Professor Louise Koelmeyer is the Director of ALERT and an occupational therapist and lymphoedema practitioner with more than 30 years of working in lymphoedema assessment and management.






