The University of Texas MD Anderson Cancer Center's Research Highlights provides a glimpse into recent basic, translational and clinical cancer research from MD Anderson experts. Current discoveries include a novel target for mutant colorectal cancers, advances in breast cancer metastases to the brain and bone, a new understanding for secondary leukemias, biomarkers for myelofibrosis treatment response, a computational tool for combining single-cell datasets, unique immune features of pre-cancerous pancreatic cysts, encouraging clinical results for Ewing sarcoma and a new protein critical for T cells to mount an anti-tumor immune response.
TDO2 identified as novel therapeutic target in APC-deficient colorectal cancers
Inactivation of adenomatous polyposis coli (APC) is a critical step in the formation of many colorectal cancers (CRCs). APC deficiencies activate the Wnt signaling pathway to drive cancer progression but targeting the Wnt pathway has proven challenging. A research team led by Rumi Lee, Y. Alan Wang, Ph.D., and Ronald A. DePinho, M.D., sought to discover additional vulnerabilities to use as treatment targets for CRCs with APC deficiency. They identified tryptophan 2,3-dioxygenase 2 (TDO2) as a critical regulator of cancer cell growth that is upregulated when APC is inactivated. TDO2 activates the Kyn-AhR pathway, leading to increased glycolysis and cancer cell growth as well as the recruitment of immune-suppressing macrophages into the tumor microenvironment. Targeting TDO2 in models of APC-deficient cancer blocked cancer progression and enhanced immune profiles, pointing to TDO2 as a possible treatment target in cancers with APC inactivation. Learn more in Cancer Discovery.
Etirinotecan pegol did not improve survival for breast cancer patients with brain metastases
Brain metastases are common in patients with metastatic breast cancer and are associated with poor prognosis. Unfortunately, limited treatment options exist, and these patients typically are excluded from clinical trials studying new treatments. One of the few studies dedicated to metastatic breast cancer patients with stable brain metastases - the Phase III ATTAIN trial led by Debu Tripathy, M.D. - compared treatment with etirinotecan pegol or chemotherapy of the physician's choice. The trial enrolled 178 patients across 47 sites and 10 countries. Investigators found no statistically significant difference in outcomes between the groups. The median overall survival was 7.8 months with etirinotecan pegol versus 7.5 months with chemotherapy, while median progression-free survival was 2.8 months for etirinotecan pegol versus 1.9 months for chemotherapy. This represents one of the first and largest trials devoted to patients with breast cancer and brain metastases, and the results may help inform future studies for these patients. Learn more in JAMA Oncology.
Lenalidomide associated with TP53-mutated therapy-related myeloid neoplasms
Therapy-related myeloid neoplasms (t-MNs) are a type of secondary leukemia that can occur in cancer patients after chemotherapy or radiation therapy (CRT). The disease is often treatment resistant with survival less than one year, and there are no available approaches to prevent its development. Koichi Takahashi, M.D., Ph.D., and co-authors analyzed the association between t-MNs genotypes and prior CRT exposures in a large cohort of patients treated within a single institution. They showed that patients who received lenalidomide in the past have an increased risk of t-MNs marked by TP53 mutations. Using in vitro and in vivo mouse models, they demonstrated that treatment with lenalidomide, but not pomalidomide, promotes selective outgrowth of T53-mutant hematopoietic stem cells (HSCs). These results are critical to understanding the development of t-MNs and suggest that the risk of disease in patients with TP53-mutant HSCs may be mitigated by using pomalidomide over lenalidomide. Learn more in Blood.
Biomarker analysis of navitoclax plus ruxolitinib potentially useful to patients with myelofibrosis
Myelofibrosis is an aggressive myeloproliferative neoplasm that can turn into leukemia. JAK inhibitors, including ruxolitinib, have been effective in reducing enlarged spleens and improving other common symptoms in patients with myelofibrosis, but they have had limited effects in reversing bone marrow fibrosis. A primary analysis of the ongoing Phase II REFINE trial showed that the addition of navitoclax to ruxolitinib reduced spleen volume by ≥35% and reduced symptoms in a subgroup of patients with myelofibrosis no longer benefiting from ruxolitinib alone. In this exploratory biomarker analysis of the cohort, led by Naveen Pemmaraju, M.D., researchers found that patients with improvements in bone marrow fibrosis and reductions in the frequency of mutant alleles had improved overall survival compared to those without these responses. The results suggest that these biomarkers may be useful for identifying disease modification effects achieved by adding navitoclax to ruxolitinib and that this combination could be effective for patients with myelofibrosis. Learn more in The Lancet Haematology.
Study clarifies molecular pathways driving breast cancer bone metastases
Bone metastases occur in more than half of late-stage breast cancers, leading to significant pain and health complications. Unfortunately, there are no curative therapies available for treating bone metastases. The EZH2 protein, responsible for epigenetic modifications, is correlated with breast cancer bone metastasis, but its role in regulating this process was not understood. New research led by Lin Zhang, M.D., Ph.D., Jingkun Qu, M.D., Ph.D., and Dihua Yu, M.D., Ph.D., discovered that EZH2 promotes breast cancer bone metastasis in a mechanism independent of its epigenetic functions. The research team demonstrated that EZH2 increases expression of integrin β1 (ITGB1), leading to downstream activation of focal adhesion kinase (FAK) and the TGFβ signaling pathway. In laboratory models, targeted therapies to inhibit FAK were effective in blocking breast cancer bone metastases. The findings suggest FAK may be a novel therapeutic target to treat EZH2-driven breast cancer bone metastases. Learn more in Nature Communications.
Computational approach allows optimal integration of multiple single-cell datasets
Single-cell profiling technologies allow scientists to analyze DNA, RNA and protein information from many individual cells within a tumor sample to gain a clearer understanding of the many cell types present. Despite many advances in recent years, integrating single-cell data generated by multiple different technologies from the same sample remains challenging. Therefore, a research team led by Jinzhuang Dou, Ph.D., Shaoheng Liang and Ken Chen, Ph.D., developed a new mathematical solution and computational tool to better integrate and align information from disparate sources of single-cell data. Their approach, called bi-order canonical correlation analysis (bi-CCA), is designed to optimally align the rows and columns of data generated by two different experiments into a single matrix suitable for downstream analysis. The researchers validated the approach on several datasets to demonstrate the feasibility of its use. Learn more in Genome Biology.
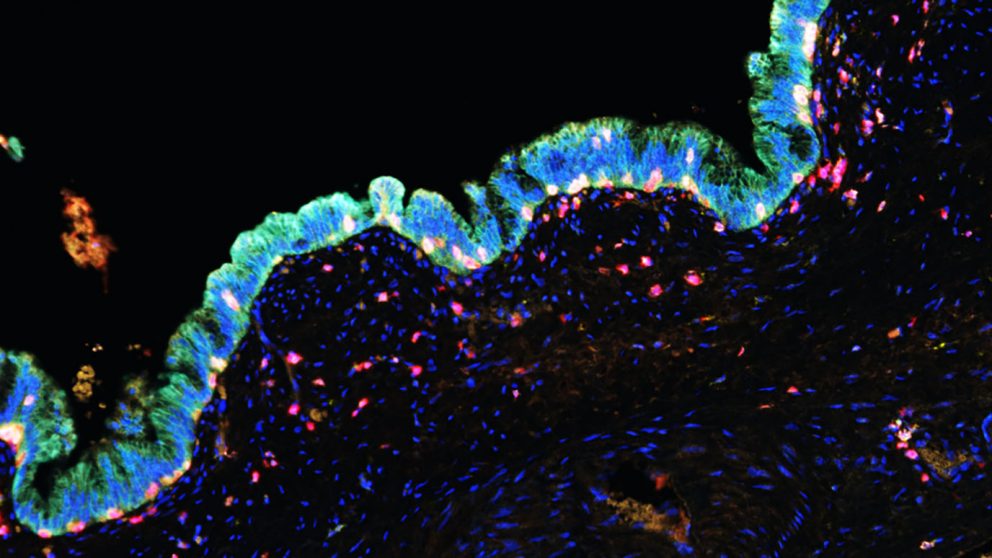
Study identifies unique immune features of pre-cancerous pancreatic cysts
Intraductal papillary mucinous neoplasms (IPMN) are pancreatic cysts that can develop into pancreatic cancer. It is important to understand which cysts are likely to progress so physicians may intervene with surgery or other treatments. Although genetic abnormalities in these cysts have been well studied, little was known about changes within the immune microenvironment. Sharia Hernandez, M.D., Edwin R. Parra Cuentas, Ph.D., Luisa Solis Soto, M.D., Subrata Sen, Ph.D., and colleagues analyzed more than 120 surgically removed IPMN samples to identify and validate immunologic features of high- and low-risk cysts. They discovered that high-grade IPMN were marked by signs of an impaired immune response relative to low-grade IPMN. Interestingly, low-grade IPMN that later progressed to cancer resembled the features of high-grade samples. These findings provide a basis for identifying high-risk IPMN, offering the opportunity to study cancer interception strategies. Learn more in Clinical Cancer Research.
Selective inhibitor of oncogene transcription shows encouraging results in Ewing sarcoma treatment
Ewing sarcoma (ES) is the second-most common malignant bone tumor in children, adolescents and young adults. Because there is currently no approved treatment for relapsed ES, developing a therapeutic agent to treat these patients is an urgent clinical need. In an open-label, Phase II basket trial, Vivek Subbiah, M.D., and researchers evaluated the safety and efficacy of lurbinectedin, an FDA-approved drug for metastatic small cell lung cancer, in 28 patients with ES. Confirmed responses were observed in four patients (14.3%), with a median duration of 4.2 months. In addition, 39.3% of patients achieved clinical benefit of either response or disease stabilization and 57.1% experienced disease control. Ten patients (40%) showed objective tumor shrinkage. The most common grade 3/4 adverse events included neutropenia (57%), anemia, thrombocytopenia and treatment-related febrile neutropenia (14% each). The findings show that lurbinectedin achieved encouraging antitumor activity with a manageable safety profile. The drug is currently being evaluated in combination with irinotecan in advanced ES in a Phase Ib/II trial. Learn more in Clinical Cancer Research.
Immunotherapy study finds critical role for BHLHE40 in anti-tumor immune response
Immune checkpoint inhibitors generate robust and durable responses in many patients with cancer, but not all benefit. Understanding factors that influence treatment responses is a major focus in the immunotherapy field. New research from the laboratory of Matthew Gubin, Ph.D., led by Avery Salmon and Alexander Shavkunov, Ph.D., demonstrated that the transcription factor BHLHE40 is crucial for T cells to mount an effective anti-tumor response following anti-CTLA-4 and anti-PD-1 checkpoint blockade. Treatment with anti-CTLA-4 or anti-PD-1 resulted in increased levels of BHLHE40 within T cells, leading to tumor microenvironment remodeling and activation of specific signaling pathways. BHLHE40 deficiency led to elevated expression of the suppressive immune receptor TIGIT, reduced expression of the cytokine IFN-γ, altered expression of metabolic genes and poor responses to checkpoint inhibitors in preclinical models. The findings suggest BHLHE40 is essential for effective immunotherapy and may be a useful biomarker to evaluate for predicting patient responses. Learn more in Cancer Immunology Research.
In case you missed it
Read below to catch up on recent MD Anderson press releases.
- Adolescent and young adult leukemia survivors have shorter life span compared to those who have never had cancer
- TJ Gan, M.D., to join MD Anderson as Division Head of Anesthesiology, Critical Care and Pain Medicine
- Targeting interleukin-6 could help relieve immunotherapy side effects