Tuberculosis (TB) is an infectious disease which has been taking a terrible toll for decades.
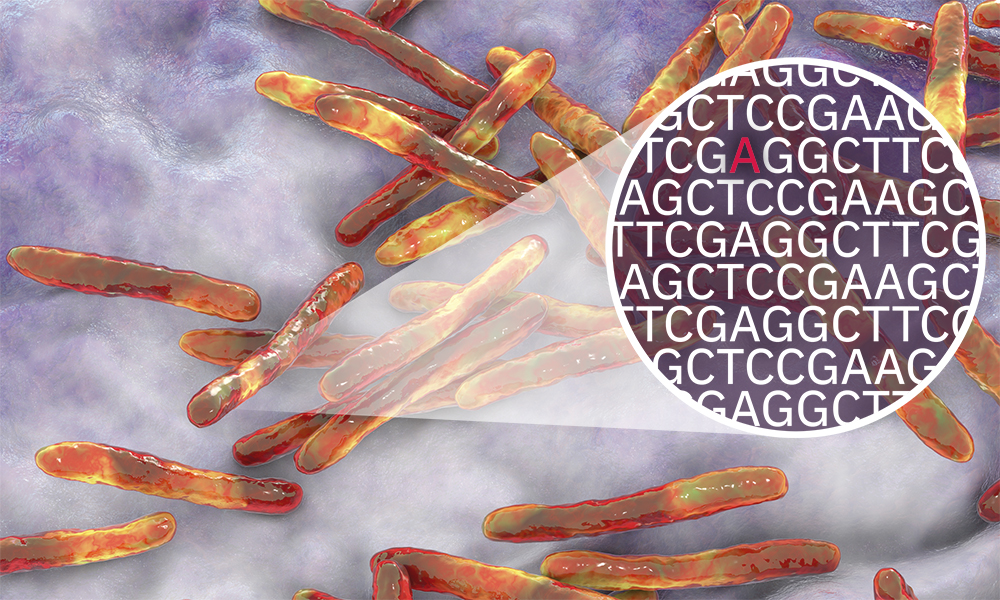
There are over 10 million cases per year and around half a million of these are caused by drug-resistant strains of the causative bacteria, Mycobacterium tuberculosis. The ongoing emergence of new mutations which cause resistance, and their spread, is a major threat to global public health.
A massive analysis of more than 10,000 different M. tuberculosis bacteria isolates from 23 countries has revealed new genes associated with resistance to 13 first- and second-line new and repurposed antibiotics.
The work, carried out by Comprehensive Resistance Prediction for Tuberculosis: an International Consortium (CRyPTIC), including EMBL-EBI researchers, is described in two new papers published in PLOS Biology.
Testing for drug resistance
In the first new paper, the researchers outlined how they assembled an open-access data compendium of 12,289 M. tuberculosis isolates, processed in CRyPTIC partner laboratories around the world. Each isolate was sequenced, and then tested on a high-throughput grid with varying concentrations of 13 antimicrobials. Of the samples included in the compendium, 6,814 were resistant to at least one drug.
In the second paper, the consortium presented their findings from a genome-wide association study (GWAS) using the data from 10,228 M. tuberculosis isolates. For all 13 antimicrobial drugs, the group discovered uncatalogued genetic variants associated with significant increases in the minimum inhibitory concentration - the lowest concentration of an antibiotic that stops the growth of M. tuberculosis.
Analysing this concentration, rather than a binary resistant-or-not-resistant result, allowed the identification of genetic variants that cause only subtle changes to antibiotic response that may be overcome by increasing drug dose. The researchers selected the 20 most significant genes that confer resistance to each drug and described the effect size and variations within these specific genes in more depth.
An open data resource for TB
"It has been a privilege to work with scientists all over the globe to build this open data resource," said Kerri Malone, EMBL-EBI Postdoctoral Researcher. "We have never even had binary phenotype data for all drugs for all isolates in a large dataset, let alone quantitative measurements, so this is a huge step. We can already see this gives us much better resolution on how some mutations increase the level of resistance more than others. This is going to open up so many doors in TB resistance research."
"I am delighted to see these core papers from the CRyPTIC consortium published, providing highly-curated open data for the community to build on, and opening new lines of investigation," explained Zamin Iqbal, EMBL-EBI Group Leader and CRyPTIC Co-investigator. "Looking forward, the community is alert for any growth in resistance to the new and repurposed drugs such as bedaquiline, clofazimine, delamanid, linezolid, which are critical to new therapeutic regimens. One outcome from the genome-wide association study is that going forward we really need quantitative measures of resistance where possible."






