Researchers at Karolinska Institutet have identified a new mechanism that may improve the treatment of ischemic stroke. The study, published in the Journal of Clinical Investigation, shows that the growth factor PDGF-CC and its receptor PDGFRα play a crucial role in scar formation in the brain after an ischemic stroke.
Ischemic stroke, where blood flow to the brain is blocked, affects approximately 12 million people worldwide each year. Of these, about one-third die, and another third suffer from permanent disabilities. Now, researchers have discovered that inhibiting PDGF-CC/PDGFRα signaling can reduce scarring in the brain and improve functional recovery after a stroke.
"Our results show that PDGF-CC and PDGFRα are involved in the formation of scar tissue in the brain after ischemic stroke. By inhibiting these molecules, we were able to reduce the size of the myofibroblast scar while also improving function in the mice" says Jil Protzmann, first author of the publication and postdoctoral researcher at the Department of Medical Biochemistry and Biophysics.
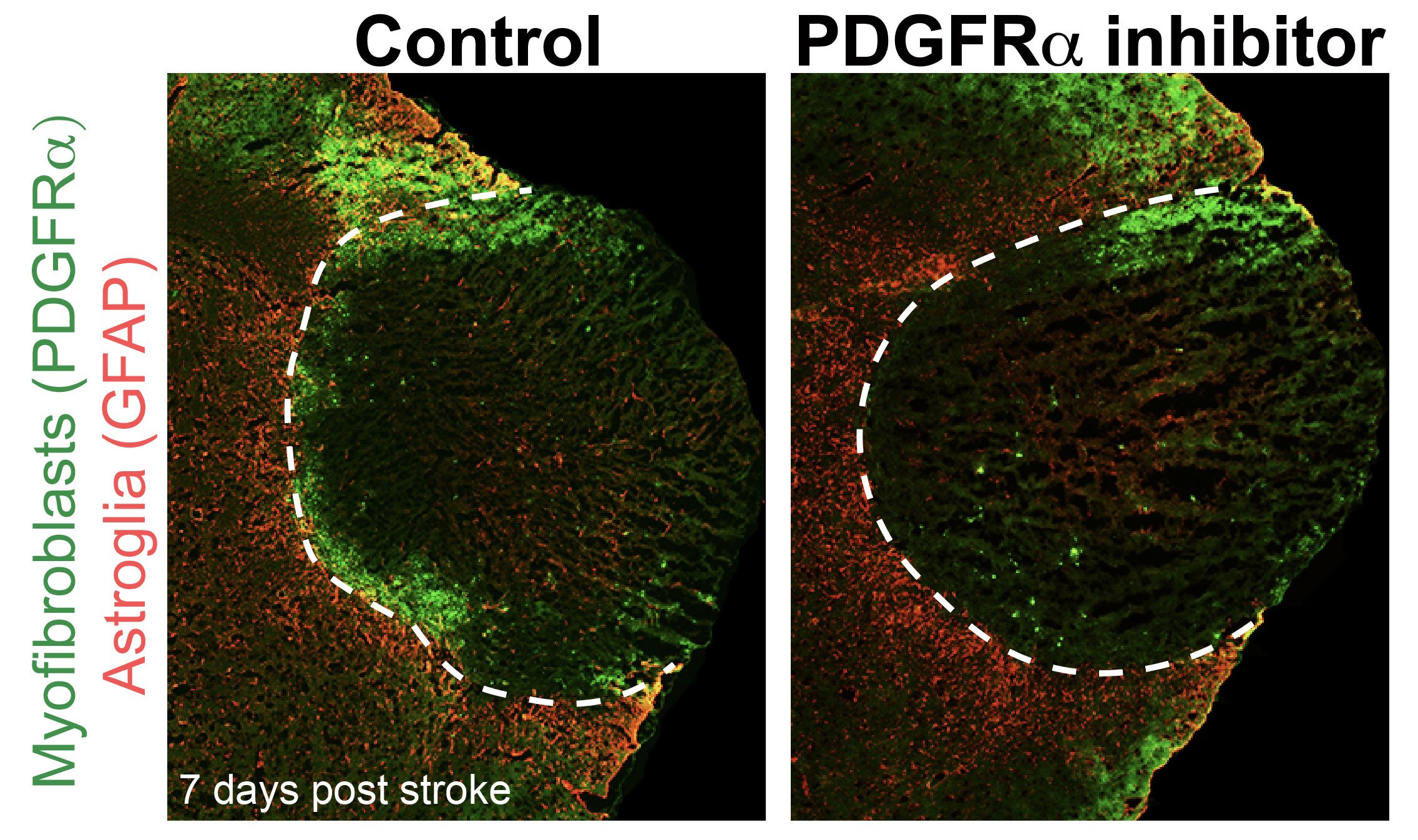

The study was conducted in mice in which an ischemic stroke was induced. The researchers used genetically modified mice and pharmacological tools, including a unique monoclonal antibody targeting PDGF-CC, to block the function of PDGF-CC and, consequently, its receptor, PDGFRα. The results showed that inhibiting PDGF-CC/PDGFRα signaling reduced myofibroblast scarring and improved the performance of mice in a behavioral test, even when treatment was initiated 24 hours after the stroke.
"This could be a new strategy for treating ischemic stroke after the acute phase, meaning days after the stroke" explains Linda Fredriksson , corresponding author of the study and researcher at the same department.
Ischemic stroke is a serious disease that places a significant burden on the affected patients, their families, and society. The only currently available pharmacological treatment is intravenous thrombolysis, which must be started within 4.5 hours of stroke onset and carries an increased risk of bleeding complications. If a patient arrives at the hospital too late, treatment options today are very limited.
The researchers now hope to translate their findings into clinical practice and investigate which brain cells are relevant for myofibroblast scarring after a stroke. They also want to determine whether inhibiting PDGFRα signaling could extend the time window for intravenous thrombolysis.
The study was funded by the Swedish Research Council, the Swedish Brain Foundation, the FGS FANG Foundation, the Ulla Hamberg Angeby and Lennart Angeby Foundation, and Karolinska Institutet. The researchers also collaborated with Professor Daniel A. Lawrence's research group at the University of Michigan Medical School, Ann Arbor, Michigan, USA.
Publikation
Protzmann J, Zeitelhofer M, Stefanitsch C, Torrente D, Adzemovic MZ, Matjunins K, Randel SJ, Lewandowski SA, Muhl L, Eriksson U, Nilsson I, Su EJ, Lawrence DA, Fredriksson L
J Clin Invest 2025 Jan;135(5):






