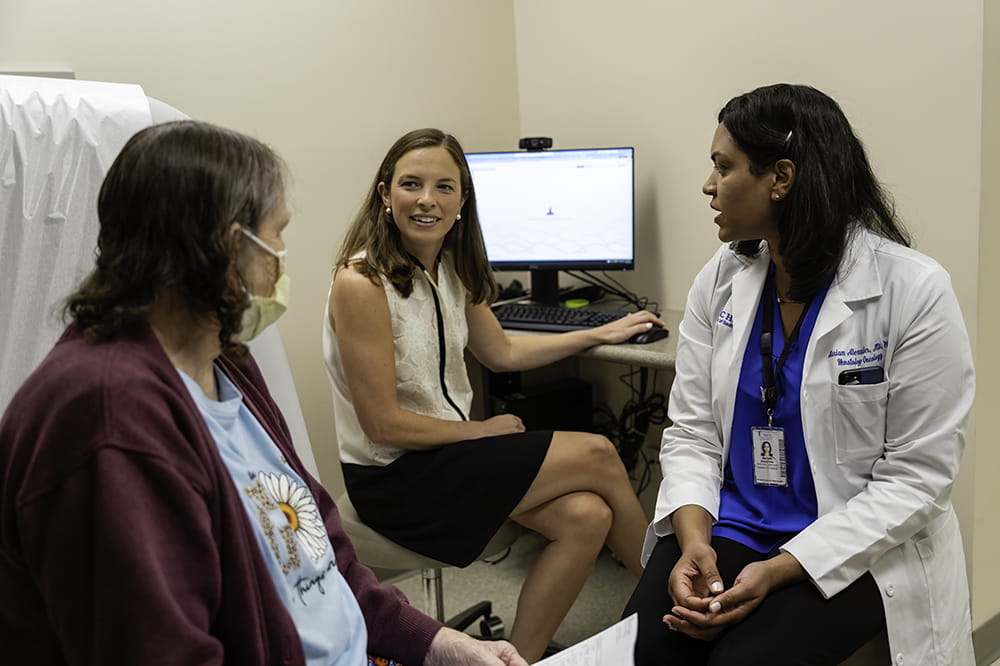
A new type of treatment for small cell lung cancer is now offered at MUSC Hollings Cancer Center, and oncologist Mariam Alexander, M.D., Ph.D., is excited not only for what this means for her patients but what it portends for treatments of solid tumors of all types.
The U.S. Food and Drug Administration approved tarlatamab in May for patients whose extensive small cell lung cancer has not responded or stopped responding to chemotherapy.
It's a bi-specific T-cell engager, or BiTE, a type of targeted therapy that looks for two targets: with one arm, it grabs onto a T-cell, a type of immune cell, and with the other arm, it attaches to a cancer cell, bringing the two cells closer together so that the T-cell can better recognize and kill the cancer cell. Up to this point, BiTE therapies have been approved only for blood cancers.
"It will be incredible to have more drugs of this nature, which is where the oncology solid tumor field is moving," Alexander said.
Hollings treated its first patient with the newly approved drug in July, but this was not the first patient at Hollings to receive tarlatamab.
Hollings participated in an arm of the clinical trial of tarlatamab, with Alexander serving as the site lead. She was impressed with the outcomes that she saw.
Small cell lung cancer
Small cell lung cancer is a difficult cancer to get under control. It's less common than non-small cell lung cancer, accounting for only about 10% to 15% of all lung cancers. But it's also a very fast-growing cancer.
"It will be incredible to have more drugs of this nature, which is where the oncology solid tumor field is moving."Mariam Alexander, M.D., Ph.D.
Unlike non-small cell lung cancer, which can often be treated with surgery if it's caught at an early stage, small cell lung cancer must be treated with radiation and chemotherapy if caught at an early stage. And it's rarely caught at an early stage. More often, it's diagnosed after it has spread, and the patient must be treated with chemotherapy and immunotherapy.
"The issue with small cell lung cancer is that it responds to chemotherapy really well in the beginning, and the reason is because it's a very fast-growing type of tumor. Fast-growing tumors respond to chemo very well. However, these responses aren't durable," said Alexander, using an oncologist's term for a treatment that lasts. "Once they are off the chemo, some patients continue to respond to the immunotherapy. But most patients don't."
After about six months, small cell lung cancer tends to come back. At that point, doctors will usually turn to a different chemotherapy since re-administering the original chemotherapy rarely works. But these chemotherapies are quite toxic with many side effects, Alexander pointed out.
"What they're seeing with tarlatamab is a durable response, so the patients who are responding continue to respond for a long time, and it doesn't have the toxicities of chemotherapy," Alexander explained.
Managing a new type of treatment
Although tarlatamab doesn't have the ongoing side effects of chemotherapy, it's not completely free of side effects. And the side effects that it does have limit the types of facilities that are likely able to offer this drug.
Like CAR-T cell therapies for blood cancers, bispecific T-cell engagers can cause significant and intense short-term side effects, including cytokine release syndrome (CRS) and neurotoxicity. CRS happens when the body is suddenly flooded with an immune response. It can cause fever, low blood pressure and even trouble breathing.
The nursing staff on the HOPE Unit in MUSC Health's Ashley River Tower and the physicians on the blood cancers team are all well-versed in handling these side effects of CAR-T cell therapy.
"The HOPE nurses have been doing this for CAR-T since 2019. They're the most experienced providers in South Carolina," explained Carrie Moore, R.N., currently the Blood and Marrow Transplant program director and formerly the manager of the HOPE unit.
When Alexander initiated the clinical trial of tarlatamab at MUSC, she relied heavily on the expertise of her blood cancer colleagues along with the guidance of Moore and her team. Together, they began to develop procedures and protocols to enable the solid tumor teams to offer these types of emerging therapies, which are likely to become more common in the future.
These patients must be closely monitored, as they can become very sick very quickly, Moore said. However, those short-term side effects can be handled, and the patient usually recovers with no ongoing ill effects. Those side effects also tend to show up only during the first two infusions, so patients can expect to be admitted for the first two infusions and to receive subsequent infusions on an outpatient basis.
In fact, Alexander said, the company behind tarlatamab is launching another clinical trial, which Hollings will be part of, to see if tarlatamab should be given earlier in the course of the disease rather than waiting for chemotherapy to stop working. That trial will be on an outpatient basis because the company believes that the side effects are manageable with more supportive care. Either way, the staff will be ready.
These are exciting therapies," Moore said. "Our experience directly relates to the quality of patient care. And we'll continue to grow our solid tumor services from here."
Alexander is happy to be able to offer options to patients who didn't have many options before. Though small cell lung cancer is relatively uncommon, doctors here still see cases every month because South Carolina has higher than average smoking rates.
"It's a significant number of patients who I feel could be helped in our state," she said.






