Researchers at the Weizmann Institute of Science have identified a yeast that might be used to prevent invasive candidiasis, a major cause of death in hospitalized and immunocompromised patients. The study, published today in the Journal of Experimental Medicine (JEM), shows that the novel yeast lives harmlessly in the intestines of mice and humans, and - as has so far been shown in laboratory animals - it can displace the yeast responsible for candidiasis, Candida albicans.
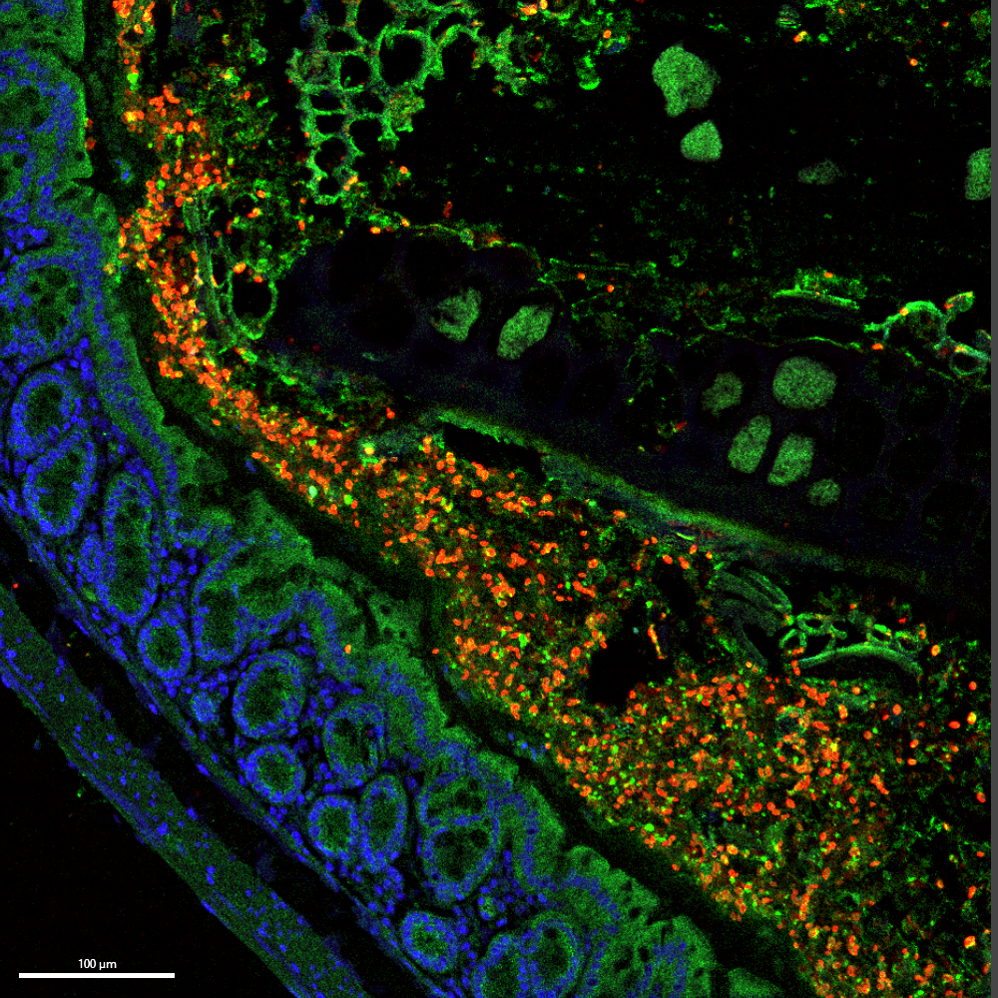
Millions of microbial species live within or on the human body, many of them harmless or even beneficial to human health. Among these are various species of yeast, which belong to the fungus kingdom. The microscopic yeast Candida albicans, commonly found in the intestines and the body's inner cavities, is usually benign, though occasionally it may overgrow and cause superficial infections commonly known as thrush. Under certain circumstances, however, the yeast may penetrate the intestinal barrier and infect the blood or internal organs. This dangerous condition, known as invasive candidiasis, is commonly seen in healthcare environments, particularly in immunocompromised patients, with mortality rates of up to 25 percent.
Like many scientific breakthroughs, this research began with a serendipitous finding. While studying yeast infections, Prof. Steffen Jung and colleagues at the Weizmann Institute noticed that some of their laboratory mice could not be colonized with C. albicans, but rather carried a previously unknown species of yeast.

"Knowing that C. albicans can cause life-threatening disease, we decided to investigate this further," Jung says. "And indeed, this line of research paid off - we found that the novel yeast could robustly prevent colonization with C. albicans."
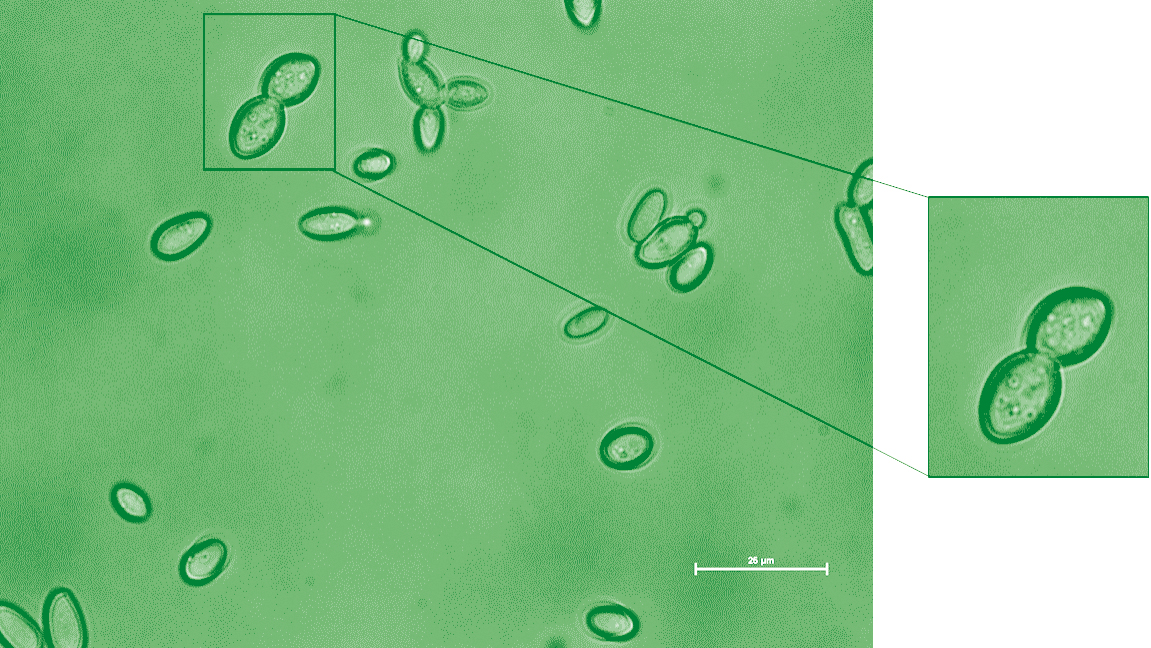
The researchers named the new species Kazachstania weizmannii, in honor of Dr. Chaim Weizmann, Israel's first president and founder of the Weizmann Institute. This species is closely related to yeast associated with sourdough production and appears to live innocuously in the intestines of mice, even when the animals are immunosuppressed.
But most importantly, the researchers found that K. weizmannii can outcompete C. albicans for its place within the gut, reducing the population of C. albicans in mouse intestines. Moreover, although C. albicans can cross the intestinal barrier and spread to other organs in immunosuppressed mice, exposure of such animals to K. weizmannii significantly delayed the onset of invasive candidiasis.
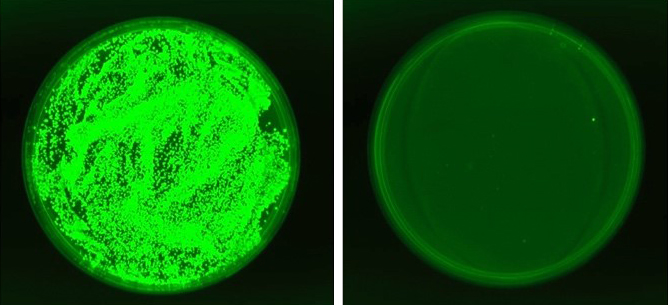
Notably, Jung and colleagues also identified K. weizmannii and other, similar species in human gut samples. Their preliminary data suggest that the presence of K. weizmannii was mutually exclusive with the presence of Candida species, suggesting that the two species might also compete with each other in human intestines, although these findings need to be substantiated by further analyses.
"By virtue of its ability to successfully compete with C. albicans in the mouse gut, K. weizmannii reduced the presence of C. albicans and mitigated candidiasis development in immunosuppressed animals," Jung says. "This competition between Kazachstania and Candida species might possibly have therapeutic value for the management of human diseases caused by C. albicans."
The study was led by postdoctoral fellow Dr. Jarmila Sekeresova Kralova and research student Catalina Donic in Jung's lab in Weizmann's Immunology and Regenerative Biology Department. Study authors also included Sebastien Trzebanski and Dr. Sigalit Boura-Halfon of Jung's lab; Dr. Ilana Livyatan, Dr. Lian Narunsky-Haziza, Prof. Eran Segal and Prof. Ravid Straussman of Weizmann's Molecular Cell Biology Department; Dr. David Zeevi of Weizmann's Plant and Environmental Sciences Department; Omer Asraf and Prof. Yitzhak Pilpel of Weizmann's Molecular Genetics Department; Dr. Bareket Dassa, Dr. Shifra Ben-Dor, Dr. Lena Fidel and Dr. Ghil Jona of Weizmann's Life Sciences Core Facilities Department; Dr. Ori Brenner, Dr. Hagit Dafni and Dr. Noa Stettner of Weizmann's Veterinary Resources Department; Dr. Neta Shlezinger of the Hebrew University of Jerusalem; Paul Mathias Jansen, Dr. Sascha Brunke and Prof. Bernhard Hube of the Leibniz Institute for Natural Product Research and Infection Biology - Hans Knoell Institute (HKI), Jena, Germany; and Prof. Petra Bacher of Christian-Albrecht-University of Kiel, Kiel, Germany.
Prof. Steffen Jung holds the Henry H. Drake Professorial Chair of Immunology. His research is supported by the Sagol Institute for Longevity Research and the Morris Kahn Institute for Human Immunology.






