Gita Fulwiler had always been an early riser -- up and moving at the crack of dawn.
But in June 2023, she started struggling to get out of bed. She constantly felt tired and out of breath after walking just a couple of steps. Making her bed felt exhausting, like running a marathon.
Fulwiler's cardiologist worried she might have coronary artery disease, also known as CAD, so her they ordered a computerized tomography (CT) coronary angiogram to check for blocked arteries.
To their surprise, the CT results did not show any blockage but instead detected a congenital heart defect — despite Fulwiler being in her early 60s.
Normally, congenital heart defects are diagnosed during pregnancy or after birth, oftentimes because of obvious symptoms such as bluish skin, fatigue, a heart murmur or fast breathing.
"I have always been a high-energy and active person," shared Fulwiler. "I couldn't believe this was something that went unnoticed for so long."
A rare congenital heart defect
Fulwiler's cardiologist referred her to UC Davis Health where she underwent a heart ultrasound, known as transthoracic echocardiogram (TTE). The procedure is a noninvasive way to look at blood flow through the heart and its valves.
The TTE revealed a congenital heart defect where there's a hole in the wall between the heart's upper chambers, and some of the blood vessels of the lungs are attached to the wrong place in the heart. In medical terms, the defect consisted of a rare form of atrial septal defect (ASD) known as a sinus venosus ASD associated with partial anomalous pulmonary venous return (PAPVR).
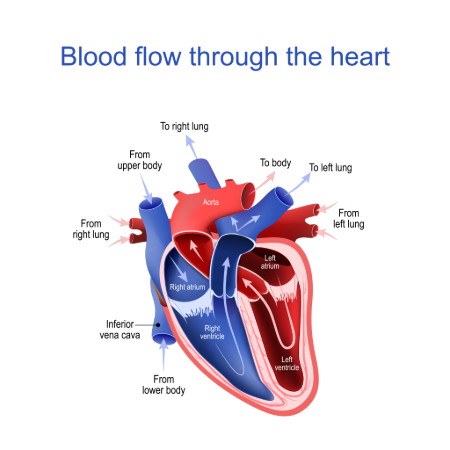
In a typical heart, oxygen-rich blood returns from the lungs to the upper left heart chamber, called the left atrium via the pulmonary veins. This blood is then pumped to feed the body.
In PAPVR, blood flows from the lungs into the upper right heart chamber, called the right atrium, and then goes back to the lungs. This oxygen-rich blood goes back to the lungs rather than feed the body, which prompts shortness of breath or fatigue.
In addition to the PAPVR, Fulwiler also had the sinus venosus ASD, a hole between the right atrium and the left atrium, which also contributes to the abnormal flow of oxygen-rich blood from the left atrium back into the right atrium. The two defects combined result in severe inefficient pumping of extra blood flow back to the lungs without contributing to oxygenation of the body.
Standard treatment of a sinus venosus ASD with PAPVR is open heart surgery, which repairs the defect and redirects the anomalous pulmonary veins back to the left atrium. Most of these lesions are diagnosed and repaired as a child. However, doctors were concerned about Fulwiler undergoing surgery, which could be considered high-risk due to her chronic pre-existing conditions that included diabetes, rheumatoid arthritis and eosinophilic asthma.
An alternative to surgery
To explore a minimally invasive alternative to surgery, Fulwiler met with interventional cardiologist Frank Ing, chief of pediatric cardiology at UC Davis Health. Though an adult, Fulwiler saw Ing because adult cardiologists are not trained to treat congenital heart defects.
"Dr. Ing sat with me for a long time, sharing a great amount of detail on how he could treat my condition," shared Fulwiler. "He showed me diagrams and walked me through the whole process."
Ing explained they would first need to close the ASD by implanting a large, covered stent anchored in the superior vena cava and extending down to the ASD. But it was not as simple as just plugging up a hole. They needed to cover the hole but also allow blood from the anomalous pulmonary veins to return properly to the left atrium.
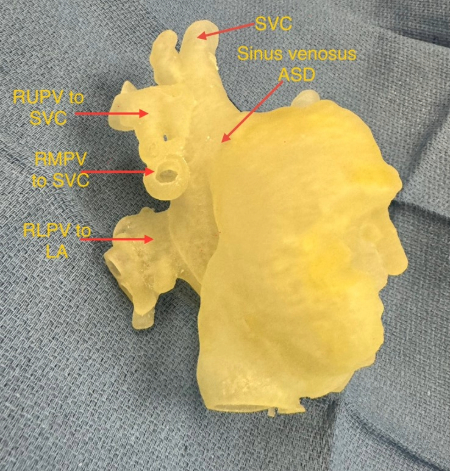
Ing also noticed two of Fulwiler's three major branches of the right pulmonary vein (each with two major vessels) were abnormal. Based on the CT scan and a 3D model of her heart, Ing explained that the most superior of the pulmonary vein branch was simply too high up and there was no way he could redirect that one branch to the left atrium. While the lowest pulmonary vein branch was not a problem, the two middle pulmonary veins were worrisome.
"The goal of the procedure is to redirect blood flow as normal as possible," explained Ing. "In this case we knew one vein could not be redirected normally and one vein could be. With the other middle two branches, we did not want to redirect them unless we knew we could successfully do so without obstructing blood flow back to the left atrium."
Use of VR technology
To test if he could successfully redirect the two middle pulmonary veins, Ing utilized virtual reality, a novel technology being used at UC Davis Health.
Through augmented reality goggles, Ing was able to project 3D computed tomography (CT) and MRI scans of Fulwiler's heart and overlay this critical information directly into his field of view.
"Using the goggles, I was able to see the anatomy of Gita's heart and simulate a stent in place to see if there would be a potential obstruction," Ing said. This simulation exercise indeed showed potential obstruction when the stent was placed into position.
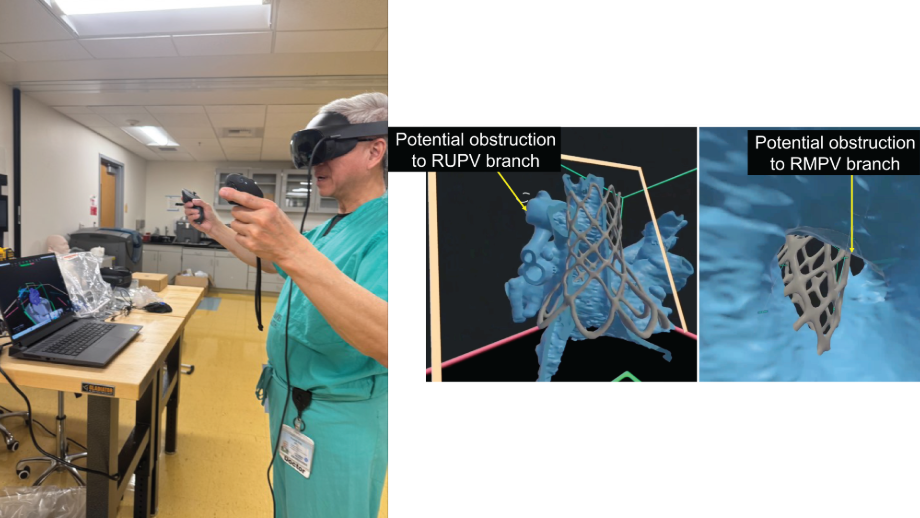
To avoid this problem, Ing inflated two high-pressure balloons in the middle of two pulmonary veins. Then he implanted the covered stent under low pressure. Because of the two different states of pressure, the two high-pressure balloons prevented the stent from encroaching the opening of the veins. This allowed the stent to mold to the shape of the two balloons.
"In the end, we were able to successfully close the hole in her heart and allow the two middle pulmonary veins that were in question (plus the lowest pulmonary vein) to get flow to the left atrium without any obstruction," Ing shared.

Back on track
Fulwiler came out of the procedure feeling great. Just a few weeks later, she was already walking 30 minutes each day on the treadmill and lifting some light weights.
"My quality of life was really declining before my procedure," shared Fulwiler. "I now feel like myself again and so appreciative to Dr. Ing and his entire team for helping me feel this way."






