Key takeaways
- UCLA researchers have identified type 5 collagen as a key factor in kidney fibrosis, revealing its potential as a biomarker to predict chronic kidney disease progression.
- A repurposed anti-cancer drug, Cilengitide, was found to reduce kidney scarring and slow disease progression in preclinical models, suggesting a possible precision medicine approach for high-risk patients.
- The team now seeks to develop a blood test to measure type 5 collagen levels, which could help identify patients at greater risk for kidney failure and guide targeted treatment strategies.
New UCLA research conducted using mouse models and human genetic data has uncovered a critical factor that determines how much scarring occurs following kidney injury, leading scientists to identify a potential precision medicine approach to prevent chronic kidney disease progression.
The study, published in Science Translational Medicine, highlights the role of type 5 collagen — a minor component of scar tissue — in kidney fibrosis, and shows how an experimental therapy could help prevent kidney failure in high-risk individuals.
Chronic kidney disease is a progressive condition that can result from diabetes, high blood pressure and kidney stones, among other causes. It affects more than one in seven adults in the United States and 800 million people worldwide. As it advances, excessive fibrosis or buildup of scar tissue impairs the ability of the kidneys to filter toxins from the blood and reabsorb water, often leading to kidney failure. There are currently no therapies that directly target or reverse this process, requiring patients to undergo dialysis or organ transplantation.
"Fibrosis, or scarring, is one of the strongest predictors of kidney failure, but it has not been clear why some people develop more extensive kidney scarring than others," said Dr. Arjun Deb, the study's senior author and a member of Eli and Edythe Broad Center of Regenerative Medicine and Stem Cell Research at UCLA. "Our findings indicate that differences in type 5 collagen expression help explain this variation and that testing for expression of this gene or protein could identify people at greater risk."
This work was funded by the National Institutes of Health, the Department of Defense, and the California Institute for Regenerative Medicine.
How type 5 collagen determines scarring severity
In a previous study focusing on heart injury, Deb identified that mice lacking the ability to produce type 5 collagen suffered more extensive scarring after a heart attack.
To determine if these same mechanisms translated to kidney injury, Deb and his team began analyzing data from the UK Biobank, a long-term study tracking more than 1.5 million people. They discovered that expression of Col5a1, the gene encoding type 5 collagen, strongly correlated with the risk of developing chronic kidney disease over the course of a decade.
"This gave us a clue that, in humans, Col5a1 expression could potentially be used as a biomarker to identify individuals who would be more likely to progress to kidney failure," said Deb, who is a professor of medicine (cardiology) and molecular, cell and developmental biology and director of the David Geffen School of Medicine's cardiovascular theme.
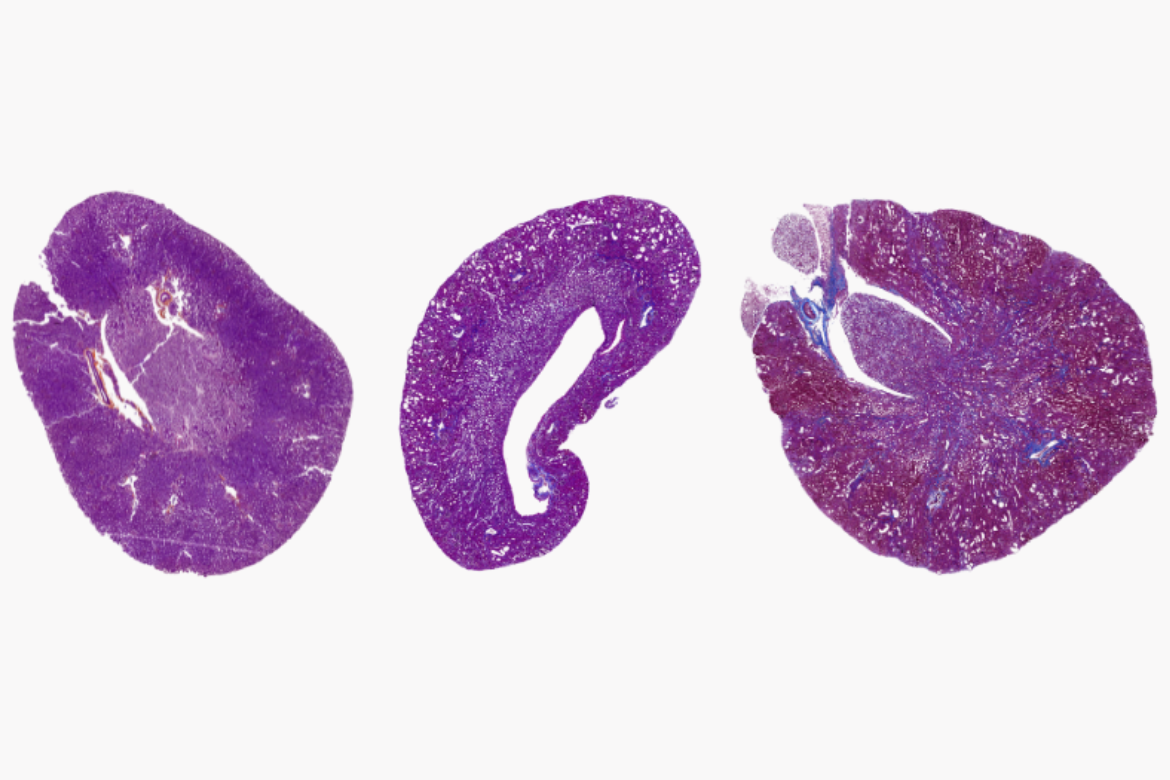
A series of experiments in mouse models confirmed these findings: Mice with low Col5a1 developed more severe fibrosis and progressed more rapidly to kidney failure following kidney injury. As with humans, type 5 collagen was playing a crucial role in maintaining the structure and function of scar tissue. Collagen fibers, Deb explained, are like the threads that hold a piece of fabric together.
"Collagens are fibrillar in nature, and they give strength to scar tissue," he said. "The way the fibers are arranged is very important. Type 5 collagen ensures the fabric of a scar is not woven haphazardly — that it is instead structured and stable."
Without type 5 collagen, the body senses that the scar tissue has formed in a weaker, more disorganized manner. This activates αvβ3 integrins — receptors in fibroblast cells that sense the weakened tissue and respond by producing even more scar tissue. This cycle of excessive fibrosis leads to worsening kidney function and, ultimately, kidney failure.
A precision medicine approach: blocking integrin αvβ3
Recognizing that excessive integrin activity was driving fibrosis in animals with decreased type 5 collagen, the team sought a way to block this pathway. They found a potential solution in Cilengitide, a drug that disrupts integrin signaling.
Originally developed as an anti-cancer therapy, Cilengitide progressed through clinical trials and was found to be safe, but ultimately not effective against cancer.
The team found that treating animals with decreased type 5 collagen with Cilengitide significantly reduced kidney fibrosis and slowed disease progression. Notably, it had no effect in mice with normal Col5a1 expression, highlighting its potential as a targeted therapy for individuals at risk of rapid disease progression.
"This presents an exciting opportunity to potentially repurpose this drug, which was already deemed safe by the FDA, for a completely different indication," Deb said.
Translating findings to clinical application
Deb's team is now working to establish a blood test to measure Col5a1 levels in human patients with chronic kidney disease to establish a clinical threshold for identifying at-risk individuals. If validated, this biomarker could be used to guide treatment decisions, pinpointing patients who could benefit from this targeted approach to slowing disease progression.
"Chronic kidney disease presents a large time window of opportunity for intervention, and you need a precision medicine approach to determine who is likely to have accelerated disease progression and require renal replacement therapies," Deb said. "We can use a simple blood test to measure type 5 collagen levels and identify individuals who could potentially benefit from this drug."
Beyond chronic kidney disease, the researchers are also investigating whether the same mechanisms contribute to fibrosis in the liver and blood vessels, where scarring is a major driver of disease.
The use of Cilengitide has not been tested in humans as a treatment for excessive scarring and has not been approved by the Food and Drug Administration as safe and effective for this use. This novel therapeutic approach is covered by a patent application filed by the UCLA Technology Development Group on behalf of the Regents of the University of California.
Other UCLA authors include Lianjiu Su, Qihao Sun, Yusheng Li, Juan Felipe Alvarez, Bo Tao, Guanglin Zhang, Yiqian Gu, Mark R. Hanudel, Alejandro Espinoza, Linlin Zhang, Calvin Pan, Shen Li, Matteo Pellegrini, Hooman Allayee, Aldons J. Lusis, James R. Hilser and Jaana A. Hartiala.






