The opioid crisis has been a major issue for health care officials across the United States.
It has also dramatically changed the treatment of chronic pain, said Adam T. Hirsh, director of the IUPUI Pain Research Laboratory and an associate professor of psychology in the School of Science at IUPUI, who is the lead author on a new study exploring racial disparities in pain care.
"Given the ongoing change in treatment, and societal attention to the opioid epidemic, it's important to understand racial disparities for pain care as they are existing in today's climate," Hirsh said.
"There's a long history of literature on racial disparities in pain care and, historically, it is focused on black patients with pain receiving fewer and less-potent opioids compared to white patients with pain," he continued.
In their study recently published in the journal Pain, Hirsh and colleagues found that white physicians who self-scored higher on "intergroup anxiety" -- discomfort during interactions with groups who share fewer similar characteristics -- were more likely to recommend opioid treatment to African American patients with chronic pain.
According to the study, white physicians with high intergroup anxiety were less likely to recommend non-opioid forms of treatment or refer African American patients to pain specialists -- recommendations that might be seen as more likely to lead to conflict or require further persuasion or explanation from the provider.
Hirsh said one reason that white providers might feel less comfortable talking to African American patients with pain is because they don't have a lot of experience interacting with people who are different from them.
"We all tend to play in the sandboxes or playgrounds with people who look like us," Hirsh said. "Self-selected segregation is still pervasive in our society. Just look at our neighborhoods in Indianapolis."
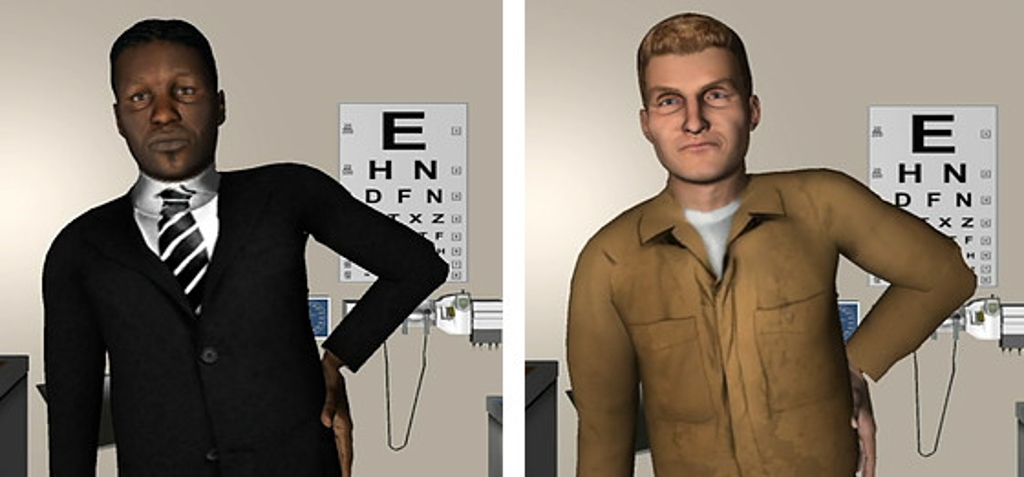
Using computer-simulated patients
Hirsh is also one of the first people to look at virtual or computer-simulated patients in the context of pain care. He has been using, creating and refining these models for over a decade.
But why use computer simulations to study such a complex and interpersonal issue?
Though he has used patient actors in past studies, Hirsh said, trying to isolate the impact of a patient's race is very difficult with real humans because the effect of their race is confounded or influenced by other factors.
"One of the challenges is to have patients demonstrate the same type of pain and communicate that pain in the exact same way, the only difference being that one patient is white and another black," he said.
By contrast, simulated patients allow Hirsh to filter out unwanted variables and gain more accurate results from his study. "That's where computer stimuli have a lot of advantages -- it lets you standardize patients across all the other characteristics but only manipulate or change the race," he said.
Hirsh also noted that the lack of human patients in the study is a reason to be cautious about drawing definite conclusions from its results, especially since this is one of the first studies to look closely at these particular relationships between patients and providers.
Different types of pain
For their study, Hirsh and his team focused on chronic lower back pain, which is the most common form of chronic pain -- defined as pain that lasts a long time and sometimes has no clear cause.
Hirsh said it is important to study chronic pain because it has been under-studied in terms of opioid prescription compared to acute pain, which is pain that stops after a short period of time, such as pain from surgery or an injury.
Previous research has shown that an African American patient experiencing acute pain -- excruciating pain from a fractured arm, for example -- is less likely to be prescribed the necessary opioids than a white patient with the same injury, Hirsh said.
Similarly, an African American patient recovering from surgery might not be given the needed amount or strength of pain medications that a white patient in the same setting would receive, he said.
Real-world applications
Hirsh said he hopes the study will impact real-world medical care by helping providers become more aware of how their comfort level with people who are different from them can impact how they treat their patients.
But helping providers become more comfortable with patients of all backgrounds is a much more complicated task, he added.
"What can we do with providers, given that we're catching them when they're 20, 30, 40, 50 years old, and we can't change their childhood?" Hirsh said.
One way to increase comfort and decrease anxiety across demographic groups might be to facilitate intergroup contact, or creating experiences for providers to work, talk with and "rub shoulders" with people who are different from them, he said.
"Just as a society, we don't have as many enriching opportunities to interact with -- on a real human-to-human level -- with people who are different than us," Hirsh said. "That's a larger societal issue that doesn't lend itself to an easy answer."
Looking toward the future, Hirsh is curious about the methodology providers use today to assess the riskiness of a patient -- that is, how likely a patient would be to misuse their prescription medications for pain.
"We have a recently completed study and a paper coming out, and then we have a couple other studies that we're planning now to better understand how providers are assessing riskiness among patients," he said.
The other authors of this study are Alexis Grant, Megan M. Miller and Tracy M. Anastas from IUPUI and Nicole A. Hollingshead from Ohio State University.






