A new study confirms that breast density plays a significant role in both the risk of breast cancer diagnosis and the sensitivity of mammography, which may affect screening practices.
The study, published in the American Journal of Epidemiology, showed that women with dense breasts had a 1.8 times higher likelihood of being diagnosed with breast cancer compared with women with less dense breasts. Additionally, when accounting for screening sensitivity, the relative risk of developing breast cancer was 1.7 times higher for women with dense breasts.
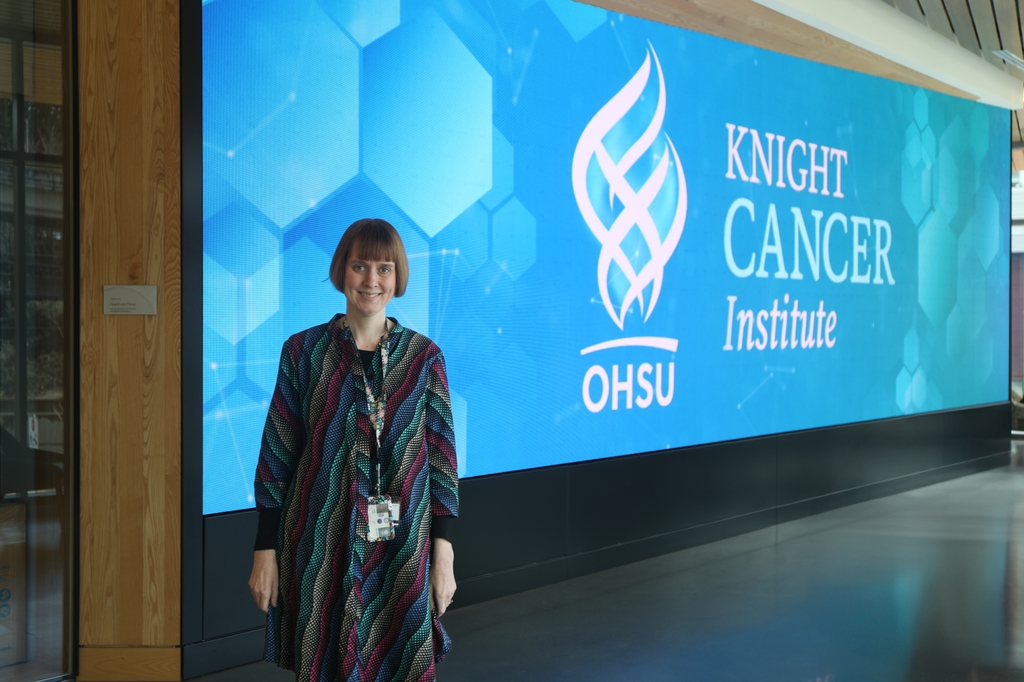
The study's lead author, Jane Lange, Ph.D., a staff scientist at the Oregon Health & Science University Knight Cancer Institute's Cancer Early Detection Advanced Research Center, said dense breast tissue not only increases cancer risk, but also makes it harder to detect tumors through routine mammograms. Breast density, which refers to the amount of fatty versus glandular tissue in the breast, has long been linked to an increased risk of breast cancer.
"Breast density has been known to be associated with an increased risk of breast cancer diagnosis," Lange said. "What we wanted to do was go beyond that and determine the actual underlying risk of developing breast cancer, separate from the biases in screening."
The study analyzed data from more than 33,000 women in the Breast Cancer Surveillance Consortium from 2000 to 2018. Researchers found that women with dense breasts were about 1.7 times more likely to develop breast cancer than those with less dense breast tissue.
Mammography is less sensitive in detecting cancer in dense breasts, leading to potential false negatives. This issue, known as "masking," may result in missed diagnoses and more interval cancers, where breast cancer is diagnosed between screenings. The study found that the sensitivity of digital mammography is 73% for women with extremely dense breasts, compared with 93% for women with mostly fatty breasts.
"Mammograms are less sensitive for women with dense breasts," Lange said. "That means tumors can be missed, leading to delayed detection. But on the other hand, women with dense breasts are often advised to get screened more frequently, which can increase the chances of finding cancer earlier."
To account for these competing factors, the researchers used a novel statistical modeling approach to separate the actual risk of developing cancer from the likelihood of detection. Their findings support recent updates to U.S. regulations requiring mammography centers to inform patients about their breast density and its implications for cancer risk.
The Food and Drug Administration has mandated that, starting in September 2024, all women undergoing mammograms must be notified if they have dense breasts and be advised of the potential risks.
"Our study really reinforces the importance of these requirements," Lange said. "Even after accounting for differences in screening sensitivity, we found that breast density is strongly linked to cancer risk."
While the study does not change current screening recommendations, Lange emphasized that women with dense breasts should be aware of their higher risk and discuss additional screening options, such as MRIs or ultrasounds, with their doctors.
"We're not making specific recommendations," Lange said. "Our study shores up the evidence that breast density is directly linked to breast cancer diagnosis and onset."
In addition to Lange, coauthors include Ruth Etzioni, Ph.D., of Fred Hutch Cancer Center, Charlotte C. Gard, Ph.D., of New Mexico State University, Ellen O'Meara, Ph.D., of the Kaiser Permanente Washington Health Research Institute, and Diana Miglioretti, Ph.D., of University of California Davis.
This study was supported by National Institutes of Health award numbers R01CA242735 and the Partnership for the Advancement of Cancer Research, supported in part by National Cancer Institute awards U54CA132383 andU54CA132381. Data collection for the Breast Cancer Surveillance Consortium was supported by funding from the National Cancer Institute awards P01CA154292 and U54CA163303, Patient-Centered Outcomes Research Institute PCS-1504 30370, and the Agency for Health Research and Quality award R01HS01836601A1. Cancer and vital status data collection was supported in part by state public health departments and cancer registries. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funders.






