Despite a record year for organ donation last year in the U.S., an estimated 17 people die every day waiting for a transplant. Yet Mayo Clinic transplant experts are optimistic that solutions to some of the biggest transplant challenges are on the horizon, thanks to new technology, research and innovations.
Watch: Dr. Burcin Taner talks about the start of organ transplant practice at Mayo Clinic
"Our goal is to transform the transplant practice for future patients. To do that, we are using technology and team science to look at ways to optimize donated organs, liberate patients from anti-rejection medications and enable donated organs to last longer," says Burcin Taner, M.D., director of Mayo Clinic Transplant Center in Florida.
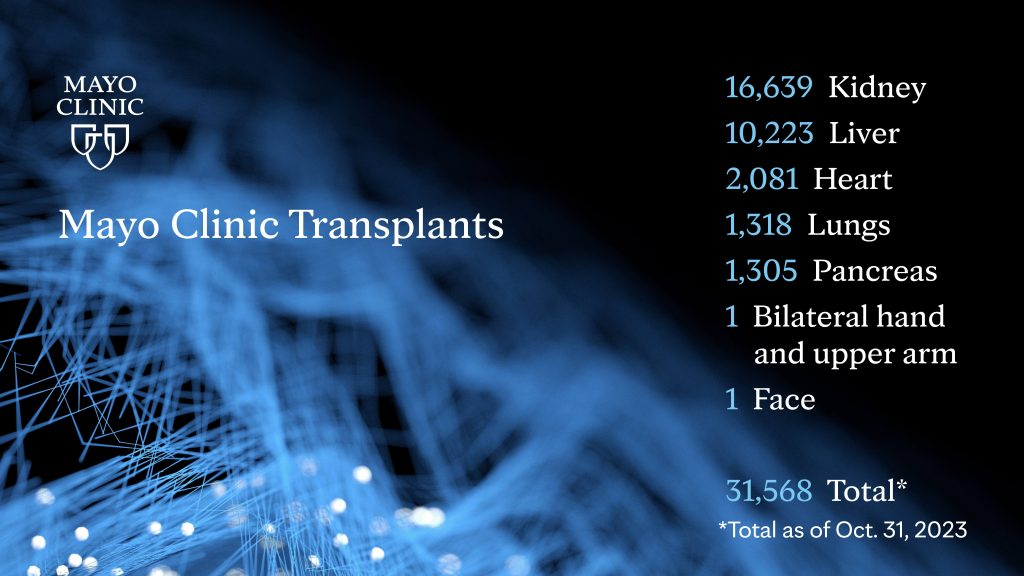
Mayo Clinic is celebrating the 60th anniversary of its first organ transplant, which was a kidney transplant from a living donor on Nov. 25, 1963. Today, Mayo Clinic is the largest integrated transplant center in the U.S. Mayo Clinic's transplant centers in Arizona, Florida and Minnesota combined have performed over 31,000 organ transplants.
"From the very beginning, organ transplantation has been exciting because it can allow a patient who has end-stage organ failure and who is extremely ill and suffering to get back to a normal life. We need to achieve that for more patients," says Julie Heimbach, M.D., director of Mayo Clinic Transplant Center in Minnesota.
Watch: Dr. Julie Heimbach talks about new advancements
Here are four promising ways transplant is changing:
1. Enabling more donated organs to be safely used.
New technology is helping ensure that more donated organs can get to the people who desperately need them. One of the biggest advances has been organ-perfusion systems. These mechanical devices enable donated organs such as lungs, hearts, kidneys and livers to remain viable outside the body for a longer period of time so that they can be used. It also allows surgeons to restore organs that would otherwise not be safe for transplantation. "Organ perfusion technology has helped us expand the donor pool and deliver lifesaving transplants to more and more patients, all while maintaining some of the best outcomes," says Bashar Aqel, M.D., director of Mayo Clinic Transplant Center in Arizona.
2. Helping transplants last longer.
The average kidney transplant in the U.S. lasts 10 to 20 years, meaning transplant recipients are often faced with needing a second transplant. But what if those donated organs could last longer? Researchers are looking at ways to keep patients healthier so that these donated organs thrive longer. For example, one of the most common causes of kidney failure is diabetes, which is related to obesity. One innovative approach is to perform bariatric surgery ahead of the kidney transplant to reduce the chance of post-transplant diabetes. Efforts are also underway to improve how organs are matched with patients with the goal of minimizing the need for immunosuppression medication, which can have negative side effects.
3. Identifying organ failure earlier.
The quicker someone is identified as being at risk for organ failure, the sooner they can begin to receive treatment in hopes of delaying - and potentially preventing - the need for a transplant. Researchers are exploring ways to identify subtle warning signs that this is happening earlier via artificial intelligence and biomarkers in the blood.
4. Bioengineering new organs.
It may sound like science fiction, but experts hope that one day there will be a way to engineer new organs using regenerative medicine. That would eliminate the uncertainty of organ donation and long waiting lists. Those efforts are still in the early stages.
While all of these potential advances offer hope, choosing to be an organ donor is a step people can take today to help save more lives. More than 103,000 people are on the waiting list in the U.S. for a transplant, according to the United Network for Organ Sharing. Living donation allows people to donate a kidney or part of their liver to someone in need. People also can register to become a deceased donor.






