PHILADELPHIA—The self-eating process in embryonic stem cells known as chaperone-mediated autophagy (CMA) and a related metabolite may serve as promising new therapeutic targets to repair or regenerate damaged cells and organs, Penn Medicine researchers show in a new study published online in Science.
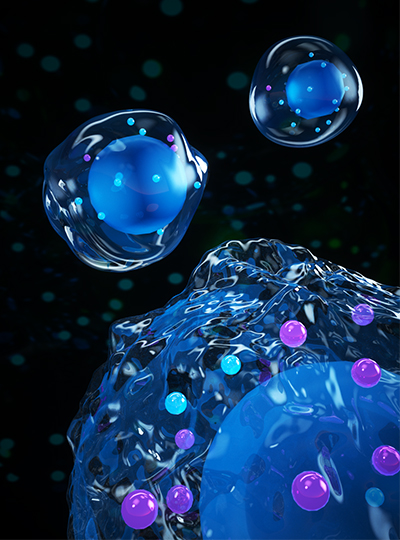
Human bodies contain over 200 different types of specialized cells. All of them can be derived from embryonic stem (ES) cells, which relentlessly self-renew while retaining the ability to differentiate into any cell type in adult animals, a state known as pluripotency. Researchers have known that the cells' metabolism plays a role in this process; however, it wasn't clear exactly how the cells' internal wiring works to keep that state and ultimately decide stem cell fate.
The new preclinical study, for the first time, shows how the stem cells keeps CMA at low levels to promote that self-renewal, and when the stem cell is ready, it switches that suppression off to enhance CMA, among other activities, and differentiate into specialized cells.
"It's an intriguing discovery in the field of stem cell biology and for researchers looking to develop therapies for tissue or organ regeneration," said senior author Xiaolu Yang, PhD, a professor of Cancer Biology at the Abramson Family Cancer Research Institute in the Perelman School of Medicine at the University of Pennsylvania. "We reveal two novel ways to potentially manipulate the self-renewal and differentiation of stem cells: CMA and a metabolite, known as alpha-ketoglutarate, that is regulated by CMA. Rationally intervening or guiding these functions could be a powerful way to increase the efficiency of regenerative medicine approaches."
Autophagy is a cell-eating mechanism necessary for survival and function of most living organisms. When cells self-eat, the intracellular materials are delivered to lysosomes, which are organelles that help break down these materials. There are a few forms of autophagy. However, unlike the other forms, which are present in all eukaryotic cells, CMA is unique to mammals. To date, the physiological role of CMA remains unclear.
Using metabolomic and genetic laboratory techniques on the embryonic stem cells of mice, the researchers sought to better understand significant changes that took place during their pluripotent state and subsequent differentiation.
They found that CMA activity is kept at a minimum due to two cellular factors critical for pluripotency—Oct4 and Sox2—that suppresses a gene known as LAMP2A, which provides instructions for making a protein called lysosomal associated membrane protein-2 necessary in CMA. The minimal CMA activity allows stem cells to maintain high levels of alpha-ketoglutarate, a metabolite that is crucial to reinforce a cell's pluripotent state, the researchers found.
When it's time for differentiation, the cells begin to upregulate CMA due to the reduction in Oct4 and Sox2. Augmented CMA activity leads to the degradation of key enzymes responsible for the production of alpha-ketoglutarate. This leads to a reduction in alpha-ketoglutarate levels as well as an increases in other cellular activities to promote differentiation. These findings reveal that CMA and alpha-ketoglutarate dictate the fate of embryonic stem cells.
Embryonic stem cells are often called pluripotent due to their remarkable ability to give rise to every cell type in the body, except the placenta and umbilical cord. Embryonic stem cells not only provide a superb system to study early mammalian development, but also hold great promise for regenerative therapies to treat various human disorders. The development of stem-cell based regenerative medicine therapies has rapidly increased in the last decade, with several approaches in studies shown to repair damaged heart tissue, replace cells in solid organ transplantation, and in some cases address neurological disorders.
"This newly discovered role of autophagy in the stem cell is the beginning of further investigations that could lead to researchers and physician-scientists to better therapies to treat various disorders," Yang said.
Penn co-authors of the study include the first author Yi Xu, a post-doctoral researcher in Yang's Lab, Yang Zhang and Sixiang Yu, also in Yang's lab, Lili Guo and Ian A. Blair of the department of Systems Pharmacology and Translational Therapeutics, Mengyuan Kan of the department of Biostatistics, Epidemiology and Informatics, as well as Juan C. García-Cañaveras and Joshua D. Rabinowitz of Princeton University.
The study was supported the National Institutes of Health (R01CA182675, R01CA184867, R01CA235760, and P30ES013508, and the Department of Defense (W81XWH-15-1-0678).






