Only one in three patients are diagnosed with broken bones in the back due to osteoporosis. One reason is that medical staff find it difficult to know who should have a back X-ray. To help address this important diagnostic care gap, academics at the University of Bristol have developed an online clinical checklist called Vfrac, to assist medical staff spot vertebral fractures that might otherwise have been missed.
The aim of this new research, published in Age and Ageing today [14 March], was to improve the clinical checklist and ensure more older women with vertebral fractures were diagnosed.
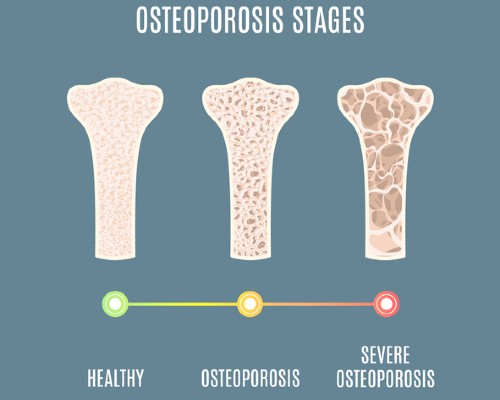
Nearly three million people in the UK have osteoporosis. Along with associated fragility fractures, osteoporosis is one of the most common musculoskeletal conditions in older people. Osteoporotic vertebral fractures (broken bones in the back due to osteoporosis) are particularly important because they identify people at high risk of future fractures.
The study, funded by Versus Arthritis, also wanted to identify the changes in prediction accuracy when including self-reported back pain, and assess the tool's potential cost-effectiveness to establish whether to test it in a real-world situation.
The Vfrac cohort study recruited 1,635 women over the age of 65 with self-reported back pain in the previous four months from nine GP practices in Bristol and 13 GP practices in Stoke-on-Trent.
Data was collected through self-completion questionnaires and physical examination including descriptions of back pain and traditional risk factors for osteoporosis such as previous fragility fractures, smoking and use of steroid tablets.
The researchers found that over 70 per cent of people with vertebral fractures were diagnosed correctly using the Vfrac checklist. This is a significant improvement compared to the current 30 per cent. Descriptions of how back pain changed with activity – particularly increasing in a crescendo of pain when standing in the kitchen leaning slightly forward, such as how people stand when washing up – improved diagnosis of vertebral fractures. Health economic analysis strongly suggests that further testing of Vfrac is appropriate.
Emma Clark, Professor of Clinical Musculoskeletal Epidemiology at the University of Bristol, Consultant Rheumatologist and Consultant Rheumatologist at North Bristol NHS Trust (NBT), who led the research, said: "Vfrac can help healthcare practitioners decide which older women attending their GP with back pain are at high risk of currently having one or more broken bones in the back due to osteoporosis and need a diagnostic spine X-ray.
"Our study found approximately one third of people recommended to have X-rays by Vfrac will have a vertebral fracture. Vfrac identified more than 90 per cent of those with severe vertebral fractures and approximately two-thirds of those with mild or moderate fractures. We now want to test Vfrac in a real-world clinic."
Angela Davies, Head of Research Engagement at Versus Arthritis, said:"We are currently starved of the diagnostic tests needed for early detection, prevention and treatment of musculoskeletal (MSK) conditions like arthritis and osteoporosis. Our research priorities and investments aim to significantly and decisively change this picture so that we can enter a world where MSK conditions can not only be treated but avoided.
"This research chimes in with our ambition. Being able to now test this tool in a clinical setting brings us a huge step closer to supporting quicker diagnoses, and ultimately better targeted treatments for people with osteoporosis."
The next steps for the research teams will be to test Vfrac with more people, particularly men, and to test it in a real-world situation such as in a clinical appointment, to find out if it works well in practice. They will also assess if it is likely to be cost-effective for use in the NHS.






