Wounds, caused by the destruction of the integrity of skins, mucosal surfaces or organ tissues, can cause severe pain to patients. Without proper care, wounds are susceptible to invasion by pathogens, causing infections and delaying wound healing. In severe cases, it can even lead to a series of complications such as tissue damage, organ failure, and septicemia.
Thus, it is essential that the wound status be monitored in a more efficient, convenient and smart manner and targeted therapy be given. Recently, the research team led by Prof. LIU Qingjun at the Zhejiang University College of Biomedical Engineering & Instrument Science developed a type of battery-free and wireless smart wound dressing for wound infection detection and on-demand drug delivery using flexible electronics. These findings were published in the journal Advanced Functional Materials.
For better skin conformity, researchers adopted serpentine wires in the electrical connection of sensing layer, which provide remarkable stretchability and biocompatibility. The sensor can take various deformations by stretching, bending and twisting, thus able to adapt to the skin and achieve direct contact with wound sites.
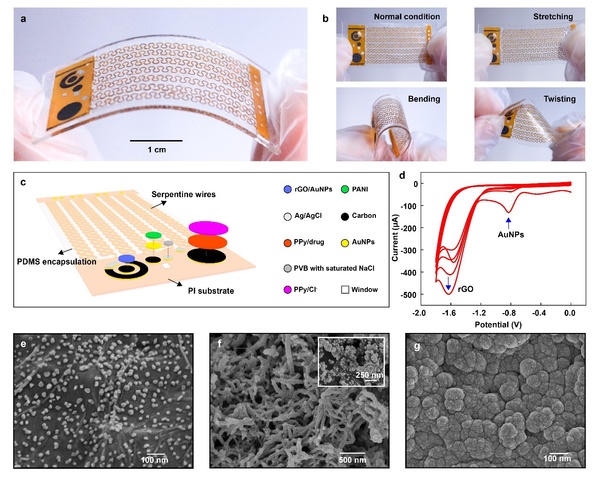
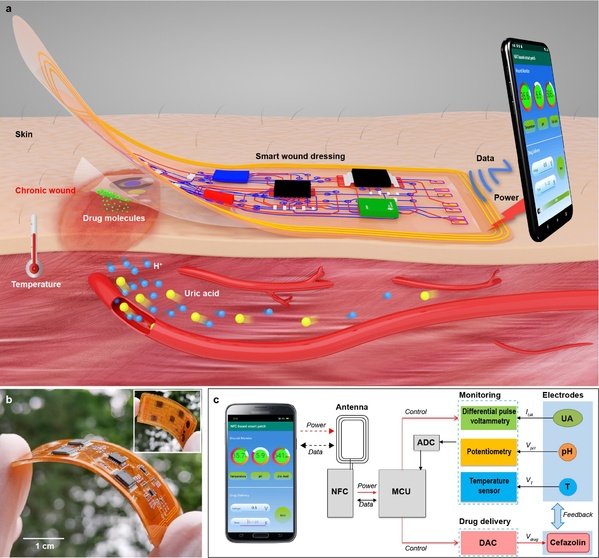
The dressing is a carefully designed double-layer patch, which includes a disposable sensing layer and a reusable flexible circuit layer. It can simultaneously detect temperature, pH, and uric acid of wounds for in situ monitoring of bacterial infections, and provide electrically controlled delivery of antibiotics for infection treatment.
"Near-field communication technology enables wireless energy harvesting to drive multiple electrochemical sensing methods for signal acquisition and wireless transmission," said LIU.
In the laboratory, no battery was found to provide power for this smart "wound dressing". Then how can power be provided? And how can information be analyzed?
These questions can be answered by a smartphone with a near-field communication (NFC) module. When the phone is close to the patch, it can achieve wireless power, obtain detection results and control drug delivery accordingly, thereby achieving a closed-loop feedback system for monitoring and drug delivery.
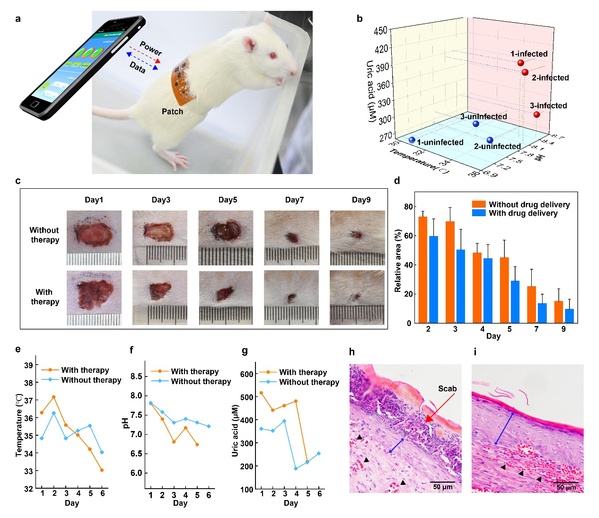
Researchers also achieved multi-parameter monitoring of wound inflammation indicators, such as uric acid, pH and temperature by means of smart sensing technology. They detected wound uric acid and pH by differential pulse voltammetry and open-circuit potentials, and monitored wound temperature using a high-precision temperature sensing chip.
According to LIU Qingjun, the results of multi-parameter wound detection can not only be used as an effective means of evaluating the degree of wound infection, but also provide guidance for electronically controlled drug delivery as a feedback assessment of drug therapeutic results.
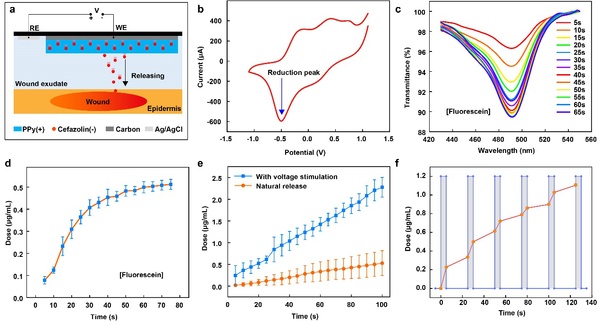
Conventional wound drug dressings are applied to the target site through the slow diffusion of the drug per se. The smart drug delivery mode developed by ZJU researchers, however, achieves precise on-demand drug delivery on the strength of electrical potential control. The electronically controlled drug delivery module uses the membrane of positively charged polypyrrole doped by negatively charged drug molecules as a coating. When a negative electrical stimulus is applied to the electrode, drug molecules will dissociate from the main chain of the polypyrrole membrane and be released to the wound site under electrical force, thereby fulfilling the purpose of treatment.
The research team expected that in the future, this miraculous "wound dressing" on the basis of near-field communication can be applied to the wearable monitoring and precise treatment of chronic wounds such as diabetic gangrene, lower limb venous ulcers, pressure sores, and severe burns, thus coming as a real boon to those suffering from long-term wound infections.






