Head and neck cancer surgeons at MUSC Hollings Cancer Center are excited about the possibilities of a new nerve fluorescing product they're testing in a phase III clinical trial.
Developed by Alume Biosciences, the product is a dye that combines a fluorescing molecule with a peptide that binds to nerves, illuminating them to make them easier for surgeons to spot.
"Taking the tumor out is easy – finding the nerve and making sure you save the nerve is the critical part. This is a trial to help determine if using this dye during surgery improves the ability of surgeons to visualize and preserve nerves," said Jason Newman, M.D., Head and Neck Cancer Division director.
Some areas of the body have more nerves than others, and the head and neck area is one where many small nerves control critical functions.
"I always tell patients, 'If we take out a tumor in your cheek, that could be a three-hour surgery. If you took the same tumor out of the skin of your back, it could be a 10-minute surgery right in the office. And the difference is that the nerve that moves your entire face is there on the cheek,'" Newman said.
Alexandra Kejner, M.D., was the first at Hollings to use the product, on a patient who needed a total thyroidectomy.
"During that surgery, we're monitoring the recurrent laryngeal nerve and the superior laryngeal nerve. These are very important for talking, singing and breathing," she said.
Currently, surgeons use electromyography (EMG) monitoring during surgery to confirm that they've reached a nerve – and that has helped to make these surgeries very safe, Kejner said.
"Still, it's confirmatory," she said. "So the thought is that with this, you may be able to preemptively identify nerves."
"Right now, we're trialing it in more straightforward cases because, theoretically, all of the nerves should be in the normal anatomic locations. But potentially, we'd be able to use these in cases where it's a revision or the third or fourth time that someone's getting a surgery in that area," she added.
When people have had multiple surgeries in the same area or if they've had extensive chemotherapy or radiation, the nerves often are no longer where they should be.
"Once you've had one surgery, the risk just multiplies," Newman said. "Especially the parotid area, if you've had one surgery there, the chance of surgery causing damage to the nerve is very high."
To use the product, patients come in an hour to five hours ahead of surgery for an infusion that lasts about half an hour.
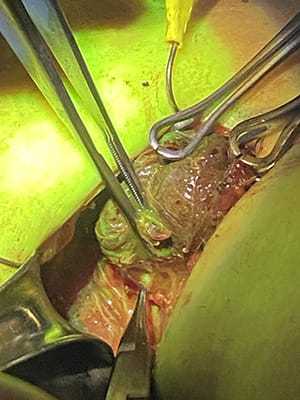
The surgeon uses surgical loupes – small microscopes attached to glasses – that are equipped with a filter that shows the fluorescence.
The dye-peptide compound binds to all nerves in the body before being flushed out through the kidneys. Newman said the dye itself has long been used in humans and is safe.
In addition to testing whether the compound improves safety, the trial is also testing the practicality of adding this product to surgery.
"It's also a feasibility study. So, 'Is it too hard for the surgeon to wear the headlamp for that long? Does the process take too long? Is it feasible for the patient to come in early for the infusion?' Also, IDS, the investigational drug supply team, has to defrost the drug and make it so we can't have the patient come in to get their surgery until at least noon because they need to prep the drug," explained Kendall Preston, the head and neck cancer study coordinator with the Hollings Clinical Trials Office.
"It does add some time to the surgery itself," Kejner said, as the lights are turned off and on to improve visualization. "But certainly anything we can do in this realm to improve our ability to do things safely is welcomed."
If approved, the product could also be beneficial for surgeons at community hospitals who don't perform these surgeries as often as surgeons at academic medical centers, Newman said.
"Part of what a good technology does is help to make everybody an expert," he said. "They take a surgeon who isn't a Dr. Kejner – who has done this a lot – and they turn that someone who has done only three of these in the last year into an expert at finding the nerve."
This would then improve safety for patients who need surgery but can't get to an academic medical center.
Newman said this is just the beginning for this type of surgical trial at Hollings.
"It's an opportunity to get the medical arts into the operating room to use cutting-edge technology," he said. "You hear about precision medicine all the time. This is precision surgery."






