Sleep has become the holy grail of health and wellbeing. But for some people, particularly shift workers and others with a chronically mistimed body-clock, getting a good night's sleep can be a constant battle that significantly disrupts their lives.
Now Flinders University researchers are moving a step closer to discovering how to personalise a sleep regime and readjust the body-clock to help treat some types of insomnia, shift work disorder and other forms of body clock disruption such as jetlag.

Led by renowned sleep and respiratory physiologist Professor Peter Catcheside, the researchers are about to begin a three-year study to develop and test a first of its kind personalised body-clock tracker to gather data to readjust the body-clock in shift-workers and those with circadian sleep disorders.
"We want to solve one of the biggest ongoing problems in sleep medicine by devising a practical way to reliably track and treat people with a body-clock timing problem," says Professor Catcheside.
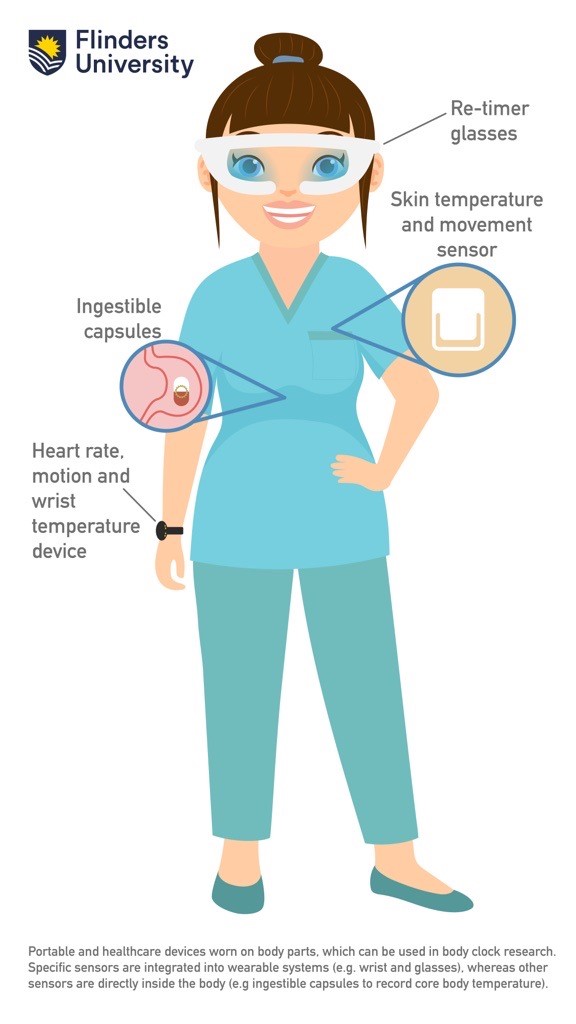
"We will use a range of technology, including heart rate, skin and core body temperature and motion monitors, in combination with physiology and engineering analysis methods, to track the daily core body temperature minimum time. This is a key marker of when the body-clock is most sensitive to re-timing effects of blue-enriched light.
"By refining and testing a first of its kind combination of high-performance wearable-sensor and circadian physiology and engineering-based analysis methods, we will be able to determine someone's individual daily light exposure timing needs for body-clock readjustment.
"Information gathered from tracking the body-clock will allow us to tailor therapies to individual shift-workers and individuals with sleep problems arising from a disrupted body-clock," he says.
The circadian system or 'body clock' plays a key role in regulating daily fluctuations in the activity of cellular and organ functions throughout the body. This complex system underpins much of our ability to perform well mentally and physically, and to sleep well.
However, with shiftwork, travel to different time-zones, and in some sleep disorders, the body-clock and wake-sleep activity cycles become disrupted.
Disruptions in the circadian and sleep systems could also play a role in chronic diseases, such as metabolic problems, heart disease, weakened immune function and a range of cognitive and mental health problems.

Professor Catcheside, who works at Flinders Health and Medical Research Institute (FHMRI): Sleep Health/ Adelaide Institute of Sleep Health, says the new project will build on recent findings from a Defence Science and Technology Group funded trial which investigated the use of smart lighting to accelerate body-clock adjustment to shiftwork.
"The body-clock senses and relays time-of-day information to the rest of the body mainly through light sensitive neural pathways from the eyes to the brain. A key result is that metabolic rate and core body temperature are normally highest when awake and lowest during sleep, in line with normal daily light-dark and activity cycles," says Professor Catcheside.
"One of the most effective ways to re-adjust the body-clock to wake-sleep schedule changes or circadian-related sleep problems is through blue-enriched light-exposure. However, the timing of therapy is critical because the body-clock is most sensitive to blue-enriched light for only a few hours a day and can be advanced or delayed depending on light exposure timing.
"Knowing when blue-light should be present versus avoided is complex and requires daily body-clock tracking and light exposure retiming tailored to each individual's shifting body-clock.
"While some wearable devices can already track skin temperature and other relevant signals, there is very limited data to support their accuracy for tracking core body temperature, especially in people with disrupted body-clocks.

"One of the main technical challenges that this project aims to solve is to develop reliable analytical methods needed to separate small circadian and sleep effects from large effects of daily activities on core body temperature and wearable sensor signals.
"We will combine wearable sensor data with high performance physiology and data-driven analysis methods to create the first practical and evidence-based daily circadian tracking method needed to optimise light therapy timing.
"With our findings we will be able to determine someone's daily adjustment of light therapy timing around their core temperature minimum to optimise body-clock adjustments using light," adds Professor Catcheside.
The Flinders team led by Professor Catcheside and other experts in sleep and circadian physiology, psychology, medicine, engineering and optometry will begin work on the project at the beginning of 2024.
The project has been awarded a $1.3 million in the latest round of National Health and Medical Research Council Ideas Grants.