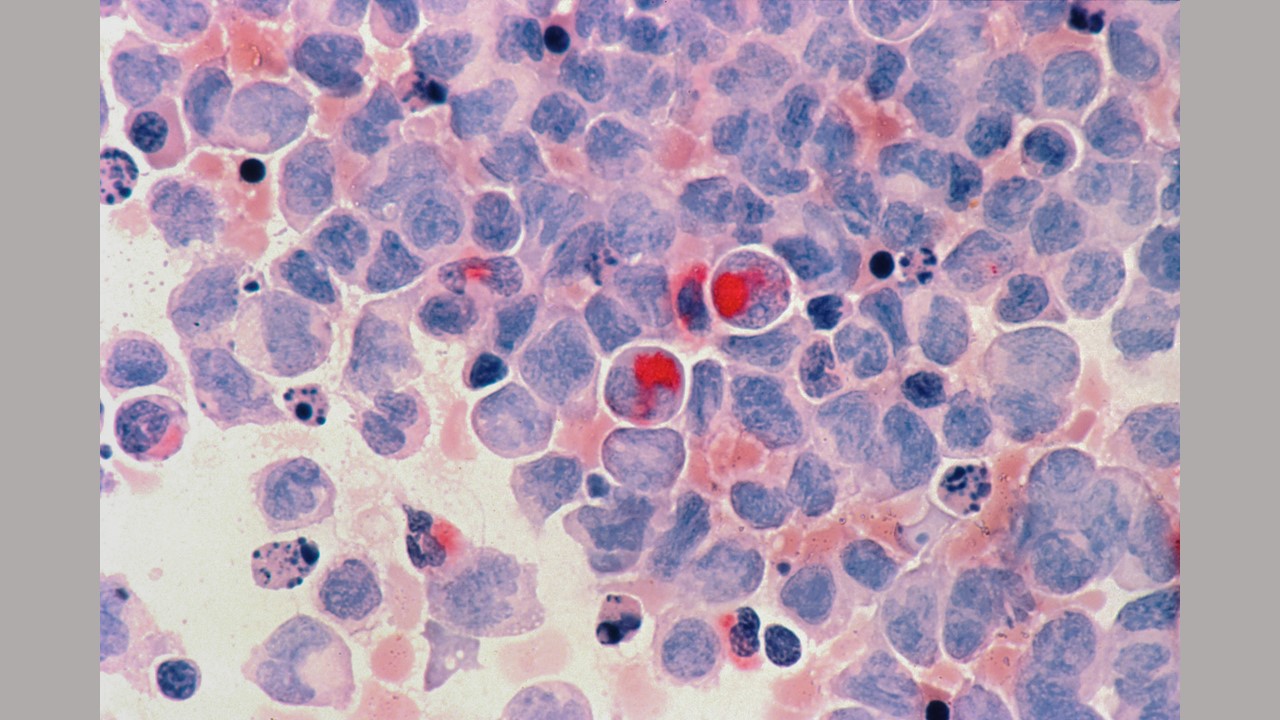
Credit: Photo by National Cancer Institute on Unsplash
Researchers from the Johns Hopkins Kimmel Cancer Center will present results from several research studies and clinical trials during the American Society of Clinical Oncology (ASCO) annual meeting, to be held June 2-6 at McCormick Place in Chicago. The meeting will bring together about 40,000 oncology professionals from around the world to discuss state-of-the-art treatment modalities, new therapies and ongoing controversies in the field.
Also at the meeting, Benjamin Levy, M.D., from Johns Hopkins, will be named an ASCO fellow, and Kellie Smith, Ph.D., and the following six oncology fellows will receive Young Investigator Awards in recognition of their research: Daniel Haldar, M.D.; Syed Hussaini, M.D.; Khaled Sanber, M.D., Ph.D.; Kara Schenk, M.D.; Yuxuan Wang, M.D., Ph.D.; and Catherine Wilbur, M.D.
Session presentations:
Saturday, June 3, Hall B1 and livestream
1:15 p.m. CDT
The ABCs of ADCs (Antibody-drug Conjugates) - This talk will cover the structure, function and role of antibody-drug conjugates for all cancers, and how these drugs work and synergize with other therapies. ADCs are an anti-cancer drug joined to an antibody (an immune system protein that targets cancer cells).
Benjamin Levy, M.D., presenter
Sunday, June 4, E350 and on demand
Patient-Reported Outcomes, Digital Health, and the Quest to Improve Health Equity - This session will highlight the challenges of expanded digital health in oncology, the value of direct patient engagement using PROs, examples of PRO implementation, and the evidence of improving cancer care delivery equity with the help of PROs.
Claire Snyder, Ph.D., session chair and presenter
Sunday, June 4, Hall D1 and livestream
11:30 a.m. CDT
Abstract #8521: Clinical Outcomes with Neoadjuvant Nivolumab Plus Chemotherapy Vs. Chemotherapy by Definitive Surgery in Patients with Resectable Non-small Cell Lung Cancer: 3-year Results from the Phase 3 CheckMate 816 Trial.
Patrick Forde, M.B.B.Ch., co-author
This abstract examines the outcomes for patients who had complete surgical resection or did not have surgery during the CheckMate 816 trial (published in The New England Journal of Medicine in May 2022), which led to the Food and Drug Administration's approval of neoadjuvant nivolumab plus chemotherapy for patients with resectable non-small cell lung cancer. This abstract suggests that while patients with resection had a better outcome, there appeared to be a benefit from adding nivolumab to chemotherapy for patients who did not have curative resection.
12:15 p.m. CDT
Abstract #8523: Response to Neoadjuvant Immune Checkpoint Inhibitor-based Therapy in Oncogene-driven Resectable Non-small Cell Lung Cancer
Samuel Rosner, M.D.
Patients who have advanced non-small cell lung cancer driven by cancer-causing genes have variable response patterns to front-line chemoimmunotherapy, leading to personalized treatment approaches based on the genetic makeup of a tumor. However, outcomes when using immune checkpoint inhibitor-based therapies prior to surgery in these patients are unknown. This study evaluated disease response and recurrence in patients with such oncogene-driven tumors that could be removed by surgery. Findings from patients treated with various immunotherapy agents suggest that recurrence-free survival is comparable regardless of the status of their oncogene drivers.
5:04 p.m. CDT
Abstract #9020: Large-scale Transcriptomic Profiling of the Tumor Immune Microenvironment in Anaplastic Lymphoma Kinase (ALK)-positive Lung Cancer
Patients with ALK+ non-small cell lung cancer do not derive significant clinical benefit from immune checkpoint inhibitor therapy. This study characterizes the major immune components of the tumor microenvironment through comprehensive transcriptomic and immunohistochemistry analyses. The findings suggest that these types of tumors have an inactive immune microenvironment, and novel strategies to enhance the immune response will be critical for improving treatment of these tumors.
Monday, June 5, Hall D1 and livestream
3:12 p.m. CDT
Abstract #9502: Nivolumab Plus Relatlimab Vs. Nivolumab in Previously Untreated Metastatic or Unresectable Melanoma: 2-year Results from RELATIVITY-047
Evan Lipson, M.D., co-author
In 2021, authors presented results from this phase III study demonstrating that in patients with previously untreated metastatic or unresectable melanoma, the immunotherapy agents nivolumab plus relatlimab improved progression-free survival versus nivolumab alone. This study provides two-year follow-up data about the durability of those responses.
5 p.m. CDT
Abstract #9506: Non-comparative, Open-label, International, Multicenter Phase I/II Study of Nivolumab ± Ipilimumab in Patients with Recurrent/Metastatic Merkel Cell Carcinoma (CheckMate 358)
Suzanne Topalian, M.D., and William Sharfman, M.D., co-authors
Researchers will present results of a multicenter global trial evaluating the immunotherapy agent nivolumab with and without ipilimumab for patients with advanced Merkel cell carcinoma - a rare and aggressive skin cancer. In contrast to recent literature, this study does not suggest an additional benefit from adding ipilimumab to nivolumab in this patient population.
Tuesday, June 6, Hall D1 and livestream
10:57 a.m. CDT
Abstract #9004: TROPION-Lung02: Datopotamab Deruxtecan (Dato-DXd) Plus Pembrolizumab (Pembro) with or Without Platinum Chemotherapy (Pt-CT) in Advanced Non-small Cell Lung Cancer (aNSCLC)
Benjamin Levy, M.D., co-author
This study evaluated the role of the antibody-drug conjugate datapotamab deruxtecan in combination with immunotherapy, and with or without platinum chemotherapy, in treatment-naïve non-small cell lung cancers. It is the first study to report on the role of any ADC as first-line treatment of patients with these cancers.
Poster abstracts:
Saturday, June 3, Hall A and on demand
• 1:15 p.m. CDT - Abstract #9552, Poster Board #315
Evan Lipson, M.D., co-author
An Indirect Treatment Comparison of the Efficacy and Safety Between Nivolumab Plus Relatlimab Versus Nivolumab Plus Ipilimumab in Advanced Melanoma, Using Patient-Level Data from the Front-Line RELATIVITY-047 and CheckMate 067 Trials
Sunday, June 4, Hall A and on demand
• 8 a.m. CDT - Abstract #9028, Poster Board #16
Joseph Christopher Murray, M.D., Ph.D.
Peripheral Myeloid Cells as Prognostic Markers in Patients with Non-Small Cell Lung Cancer Treated with Cemiplimab: A Pooled Analysis of the EMPOWER-Lung 1 and EMPOWER-Lung 3 Phase 3 Trials
• 8 a.m. CDT - Abstract #9117, Poster Board #105
Association Between Real-World, Upfront, Next-Generation Sequencing and Overall Survival in Advanced Non-Small Cell Lung Cancer in the United States
• 8 a.m. CDT - Abstract #TPS8599, Poster Board #226a
Results from the phase 3, randomized DREAM3R trial of durvalumab with chemotherapy as first-line treatment in advanced pleural mesothelioma
• 8 a.m. CDT - Abstract #TPS8604, Poster Board #228b
Patrick Forde, M.B.B.Ch., study co-author
Results From the Phase 2 NeoCOAST-2 Study of Neoadjuvant Durvalumab Plus Novel Immunotherapies and Chemotherapy or MEDI5752 (Volrustomig) Plus CT, Followed by Surgery and Adjuvant Durvalumab Plus Novel Immunotherapies or Volrustomig Alone in Patients with Resectable Non-Small Cell Lung Cancer
• 8 a.m. CDT - Abstract #TPS8609, Poster Board #231a
Benjamin Levy, M.D., study co-author
Phase 3 Trial of Durvalumab Combined with Domvanalimab Following Concurrent Chemoradiotherapy (cCRT) in Patients with Unresectable Stage III NSCLC (PACIFIC-8)
• 8 a.m. CDT - Abstract #TPS9161, Poster Board #138a
Patrick Forde, M.B.B.Ch., study co-author
Results From the Phase 3 LATIFY Study of Ceralasertib Plus Durvalumab vs. Docetaxel in Patients With Locally Advanced or Metastatic Non-Small Cell Lung Cancer that Progress While on or Following Anti-PD-(L)1 and Platinum-Based Therapy
Monday, June 5, Hall A and on demand
• 1:15 p.m. CDT - Abstract #5574, Poster Board #269
Stephanie Gaillard, M.D., Ph.D.
A Phase I Study of the Drug Fostamatinib Plus Weekly Paclitaxel for Recurrent Platinum-Resistant Ovarian Cancer
• 1:15 p.m. CDT - Abstract #TPS1616, Poster Board #206b
A Liquid Biopsy Precision Oncology Study to Evaluate the Utility of Plasma Genomic Profiling for Therapy Selection






