A multicenter safety study at UC Davis Health tested a protein drug (INBRX-101), developed to improve care for people with alpha-1 antitrypsin deficiency (AATD), and showed the therapy is quite safe.
Published in the Journal of the COPD Foundation, these results are good news for patients with AATD. This trial also sets the stage for a pivotal phase 2/3 trial, which will assess the drug's efficacy and possibly lead to U.S. Food and Drug Administration (FDA) approval.
"This is a really complex drug, and we were quite pleased the data showed it safe and tolerable," said Brooks Kuhn, associate professor of pulmonology and principal investigator on the UC Davis Health arm of the trial. "You look at the side effect profile and most of them were aches and pains. That's really exciting."
Improving on an Existing Therapy
AATD is a rare genetic disease that affects around 100,000 people in the U.S. The condition is caused by low levels of alpha-1 antitrypsin (alpha-1), an essential protein that turns down the immune response. White blood cells, called neutrophils, respond to injury and infection, but eventually, when the danger has passed, alpha-1 comes in to calm those neutrophils. Low alpha-1 mean neutrophils literally don't know when to quit, generating rampant inflammation in the lungs and other organs.
"Alpha-one is supposed to come in and tell neutrophils the war is over," said Kuhn. "But when a patient is deficient, they have unchecked, persistent neutrophilic inflammation. Because the lungs are at the front lines of exposure, they typically take the hardest hits."
AATD patients experience a variety of symptoms, including shortness of breath, chronic coughs, lung infections, emphysema, fatigue and rapid heartbeat. For the past 40 years, the standard treatment has been weekly infusions of plasma-derived alpha-1. However, the treatment can be quite onerous.
"This is one of those instances where the therapy might be almost as challenging as the actual disease," said Kuhn. "Patients must get an infusion once a week, which ends up taking half a day. For working people, it's a real challenge."
Another downside to the existing therapy is its plasma derivation. During the COVID-19 pandemic, supplies were short because people were afraid to go out and donate. This was a bad time for AATD patients, who faced a deadly respiratory virus without their normal prophylactic care.
A Sophisticated Protein Drug
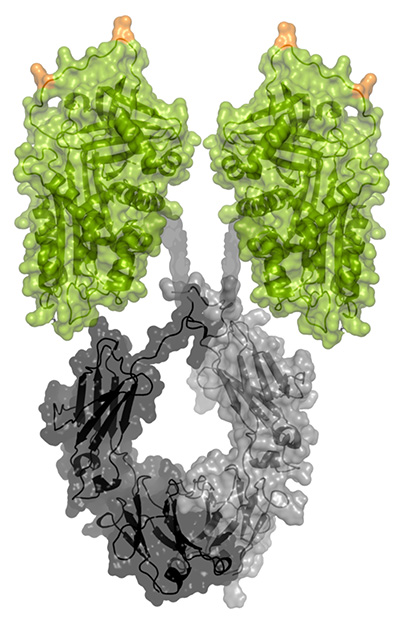
INBRX-101 was developed to help alleviate these burdens. The protein drug combines alpha-1 proteins and an antibody and is designed to stay in the blood and organs longer. Like plasma-derived alpha-1, INBRX-101 is infused regularly. However, early studies are showing this drug could potentially be given to patients every three or four weeks. In addition, because it's synthetic, this therapy could potentially reduce or eliminate supply chain issues.
The study found the drug was quite well tolerated and alpha-1 persisted in the blood for weeks. In addition, the drug maintained alpha-1 at higher levels, which could provide additional protection compared to the legacy therapy. Further study showed the drug penetrated the lungs, where it should do the most good. The drug has been given Fast Track status by the FDA, which means it could come to patients sooner.
"I was impressed by how clean the results were," said Kuhn. "The pharmacokinetics, or how long a drug is effective in the body, turned out great and the immunogenicity was minimal. There's real promise there and, for the AATD patients I treat with infusion, I don't think I can oversell the practical benefits for them."






