
At UCSF Benioff Children's Hospitals, each research paper, clinical trial and lifesaving treatment starts with a question: How can we offer hope for the future of every child?
That includes children like Gabby Lopes, who suffered a stroke at age 12 due to a rare brain disease. Gabby was rushed to UCSF Benioff Children's Hospital Oakland, where she received a novel treatment that later became the basis of the first clinical trial in the nation for acute stroke in children. Led by UCSF pediatric neurologist Heather Fullerton , MD, and spanning 25 centers across North America, the trial is bringing transformative therapy to children who might otherwise have faced lifelong disabilities, at best. Today, Gabby is back at school and playing in the band.
Every day, children like Gabby benefit from life-saving therapies discovered and tested with support from the National Institutes of Health. Last year, UCSF received $33 million in NIH awards for pediatric research across a spectrum of diseases, disorders and scientific disciplines.
"Investing in research to improve the lives of children is central to our mission here at UCSF, and NIH funding is the vital backbone that makes this care possible," said Raphael Hirsch , MD, chair of UCSF's Department of Pediatrics. "While some private foundations invest in pediatric research, they support a fraction of the need. Federal funding is one of the few places we can consistently rely on for support."
Rare immune disorders call for rare collaborations
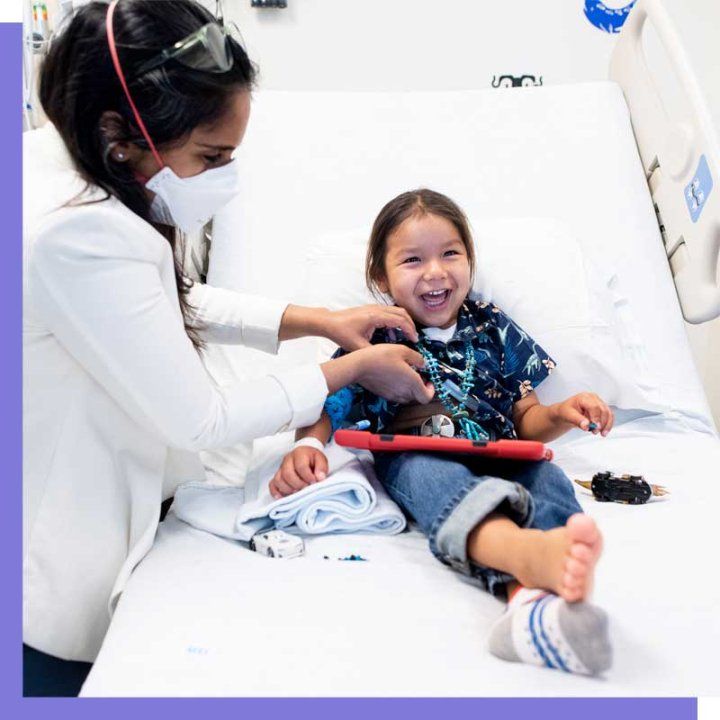
Only days after Hataalii Tiisyatonii Begay was born in Arizona, he was airlifted to Phoenix Children's Hospital and diagnosed with Artemis-SCID. Children with this condition have no immune system and usually die in the first two years of life without treatment. But UCSF researchers are leading a clinical trial for Artemis-SCID patients that enabled "HT" to become the first patient in the world to receive gene-correction therapy with his own cells - eliminating complications associated with donor cells. After successful treatment, HT is back to enjoying a normal childhood.
UCSF research: Pediatric researcher Christopher Dvorak , MD, co-leads the Primary Immune Deficiency Treatment Consortium (PIDTC), bringing together 47 centers nationwide to research and treat rare immune deficiency diseases. Dvorak's team is developing a platform to share the consortium's research, including data on severe combined immune deficiency (SCID), chronic granulomatous disease (CGD) and many other disorders, with centers across the country - ensuring patients in every state have access to cutting-edge, evidence-based care.
NIH 2024 funding: $1,815,882
Care for newborns with heart defects

By the time Brooklyn Bertilacchi hit her first birthday, she'd had four surgeries at Benioff Children's Hospitals to correct a congenital heart defect. As Brooklyn grew older, her mother, Katie, started to notice her child struggling to read and write. Katie learned that children with congenital heart disease are at an increased risk for neurodevelopmental differences such as ADHD and autism. Brooklyn and her family went back to Benioff Children's, where Brooklyn was seen in the Healthy Heart and Minds program and diagnosed with ADHD. Thanks to the decades of research into neurologic outcomes in babies with congenital heart disease, Brooklyn was connected to treatment, education, therapy and parental support that put her back on a forward path.
UCSF research: More than 40,000 babies are born with a heart defect every year. Preterm birth and congenital heart disease are two of the most common and can be life threatening. A group led by pediatric intensivist Patrick McQuillen , MD, pediatric cardiologist Shabnam Peyvandi , MD, and biomedical engineer Duan Xu pioneered neuroimaging in newborns to detect heart defects and associated brain injuries that can lead to neurodevelopmental delay and intellectual impairments. McQuillen and his team are now exploring ways to treat heart defects and prevent brain injuries before birth, aiming to eliminate developmental challenges before they even begin.
NIH 2024 Funding: $852,007
Training tomorrow's physician-researchers
Responsible patient care includes training future physician-scientists. In 2024, the NIH awarded nine grants to UCSF to mentor rising pediatricians in the fields of cancer, critical care and nutrition. One grant supports an MD/PhD student's work to advance care for children with brain-related disorders by studying the role of the blood-brain barrier in development. Another will establish a two-year post-doctoral training program in pediatric pulmonary vascular disease. By investing in budding physician researchers, UCSF ensures the best science will be translated into the best patient care for decades to come.
NIH 2024 Funding for Pediatric Training: $12,764,682 (grant range: $41,632 to $490,664)
Fullerton, Dvorak and McQuillen are among the thousands of people at UCSF whose passion and purpose are directed at the question: How can we offer hope for the future of every child?
Gabby, HT and Brooklyn are among the thousands whose lives have been changed by the research that sprang from that question.

About UCSF Benioff Children's Hospitals: UCSF Benioff UCSF Benioff Children's Hospitals are among the nation's leading pediatric specialty hospitals, according to U.S. News & World Report 2024-25 rankings. Their expertise covers virtually all pediatric conditions, including cancer, heart disease, neurological disorders, pulmonology, diabetes and endocrinology, as well as the care of critically ill newborns. The two campuses in San Francisco and Oakland are known for basic and clinical research, and for translating research into interventions for treating and preventing pediatric disease. They are part of UCSF Health, whose adult hospital ranks among the top medical centers nationwide and serves as the teaching hospital for the University of California, San Francisco, a national leader in biomedical research and graduate-level health/sciences education. Visit www.ucsfhealth.org .






